COVID-19
POCUS for COVID-19 - a review by The POCUS Atlas
Ultrasound in COVID-19
Written by Michael Macias, MD (@emedcurious), Matthew Riscinti, MD Editors: Dr. Rachel Liu, Dr. John F Kilpatrick, Dr. Tessa Damm, Dr. Tim Scheel
Last updated: June 18th, 2020 (Evidence Atlas Review)
COVID-19 Ultrasound Card
Denver Health and The POCUS Atlas have teamed up to create a COVID-19 Ultrasound protocol. These will be printed on plastic and will distributed to providers. This is FOAMED: Click to download a PDF version or contact Matthew Riscinti, MD for an Adobe Illustrator source file if you want to adapt this for your own institution. Our cleaning protocol is also available at that link.
We believe that collaboration and human-centered design will tackle the biggest problems in healthcare. The contributors to the card include, in no particular order: Matthew Riscinti, MD, Michael Macias, MD, Tim Scheel, DO, Paul Khalil, MD, Amanda Toney, MD, Molly Thiessen, MD, and John Kendall, MD.

Chest CT Findings in COVID-19
In a study by Ai et al (n=1014), chest CT was compared to RT-PCR for the diagnosis of COVID-19. Characteristic findings on CT included ground-glass opacities, multifocal patchy consolidation, and/or interstitial changes with a peripheral distribution. In patients with a positive RT-PCR, characteristic findings on chest CT demonstrated a sensitivity of 97% and specificity of 25%. In a small subset of patients with serial RT-PCR performed (initial negative followed by positive result) a positive chest CT was present PRIOR to the positive RT-PCR. Link
Image Courtesy of Dr. Marco Garrone (@drmarcogarrone)
The data on lung ultrasound in COVID-19 is limited but continues to evolve. There is already evidence on the use of chest CT in the diagnosis of COVID-19 which is what has driven many providers to turn to ultrasound as an alternative imaging option [3]. Recent studies suggests that lung ultrasound provides similar results compared to chest CT findings in COVID-19 and is superior to standard chest radiography [1]. Advantages of performing lung ultrasound over CT include: ease of use, repeatability, low cost, and avoidance of having to transport a patient with suspected COVID-19 to radiology (potentially exposing health care providers and hospital staff to unnecessary risk). The utility of bedside ultrasound in COVID-19 has not been confirmed by evidence and its role needs to be further delineated in a way that minimizes infectious risks. However, experts have proposed its importance in a variety of patient care scenarios: (1) Rapid assessment of the severity of COVID-19 at presentation (see algorithm by Dr. Mike Stone) (2) Evolution of disease (3) Monitor lung recruitment maneuvers (4) Guide response to prone position (5) Management of extracorporeal membrane therapy (6) Make decisions related to weaning from ventilatory support (7) Differentiation of shock states (including cardiogenic shock) (8) and assessment of fluid tolerance.
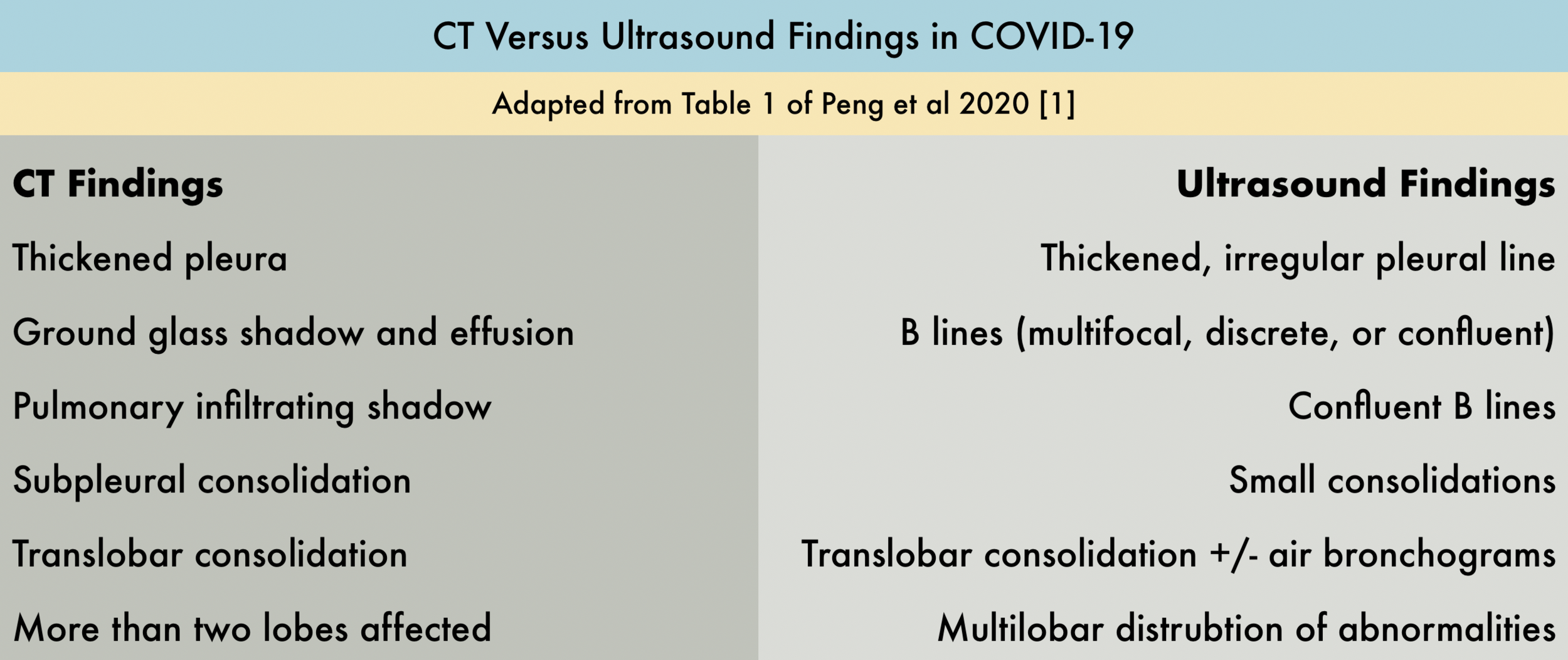
Two recent publications (Peng et al and Huang et al) have characterized important lung ultrasound findings in patients with COVID-19, review of these two publications is highly recommended if you plan on incorporating bedside ultrasound into your clinical management of suspected COVID-19 patients. Characteristic ultrasound findings compared to CT are described in the provided table. Soldati et al have proposed a standardized approach to performing lung ultrasound in patients with suspected COVID-19, including a 14-view (7 views per side) technique, and a scoring system to quantify severity of lung involvement.
A few important points to make:
Large pleural effusions are rare but small effusions can be seen around subpleural consolidations
Lesions are predominately located in the posterior lower fields of both lungs
Compared to B-lines seen in cardiogenic pulmonary edema, the B-lines seen in COVID-19 are patchy with areas of normal lung in between and are associated with an irregular pleural line with punctate defects.
The degree of lung findings appears to correlate with severity of lung injury:
Mild - Focal scattered B-lines
Progressive/Severe - Interstitial syndrome (diffuse B-lines) + lung consolidation
COVID Beyond the Lungs: Reports out of cities seeing large volumes of COVID-19 patients have reported high rates of cardiac complications including cardiogenic shock, myocarditis, and arrhythmias (Wang). It may be beneficial to approach critically ill patients with suspected or known COVID-19 as having undifferentiated shock, assessing their fluid tolerance, and evaluating for acute decompensated heart failure early in their course. There may also be a role for POCUS for confirming central lines, intubations, and ruling out a pneumothorax after invasive procedures. This may further decrease x-ray utilization and prevent contamination, staff exposure, and utilization of PPE.
Timeline of COVID-19 Lung Ultrasound Findings: A Case Study
Dr. Yale Tung Chen is an Emergency Medicine physician currently living with an active COVID-19 infection. He currently serves as the Director of the Ultrasound Division at Hospital Universitario La Paz in Madrid, Spain. He has graciously allowed us to share his #mycoviddiary on our site to help educate and provide a perspective on symptoms in comparison to lung ultrasound findings. Follow him on Twitter @yaletung!
More Images of Lung Ultrasound
COVID-19 Lung Ultrasound Findings
Normal Lung Ultrasound Anatomy
Other Lung Ultrasound Pathology
Infection Control During the COVID-19 Pandemic
EPA List of Disinfectants for Use Against SARS-CoV-2
Denver Health COVID-19 Portable Ultrasound Workflow
ACEP Ultrasound Section COVID-19 Cleaning Protocol
Using Probe Cover for Butterfly iQ + iPhone from Mike Stone
Learn More About POCUS in COVID-19
POCUS in COVID-19 via Ultrasound GEL. Michael Pratt sits down with Mike Mallin to discuss the most recent evidence regarding POCUS use in COVID-19 patients.
POCUS Use in Patients with Suspected COVID-19 via Core Ultrasound. Mike Mallin and Jacob Avila talk with Michael Prats and Mike Stone on how ultrasound can be used to help manage your patients with suspected COVID.
Comprehensive resource page on use of bedside ultrasound in suspected COVID-19 patients tailored towards Butterfly iQ use.
The Ultrasound Leadership Academy is offering a free point of care lung ultrasound learning module!
References
Peng, Q., Wang, X. & Zhang, L. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med (2020). Link
Huang, Yi and Wang, Sihan and Liu, Yue and Zhang, Yaohui and Zheng, Chuyun and Zheng, Yu and Zhang, Chaoyang and Min, Weili and Zhou, Huihui and Yu, Ming and Hu, Mingjun, A Preliminary Study on the Ultrasonic Manifestations of Peripulmonary Lesions of Non-Critical Novel Coronavirus Pneumonia (COVID-19) (February 26, 2020). Link
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology 2020. doi: 10.1148/radiol.2020200642 Link
Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585 Link
Soldati, G., Smargiassi, A., Inchingolo, R., Buonsenso, D., Perrone, T., Briganti, D.F., Perlini, S., Torri, E., Mariani, A., Mossolani, E.E., Tursi, F., Mento, F. and Demi, L. (2020), Proposal for international standardization of the use of lung ultrasound for COVID‐19 patients; a simple, quantitative, reproducible method. J Ultrasound Med. Accepted Author Manuscript. doi:10.1002/jum.15285 Link



![A COVID-19 Patient with 3 days of Symptoms [1/3]](https://images.squarespace-cdn.com/content/v1/58118909e3df282037abfad7/1584923302263-T9LBTKNFW294TEL8OU0L/ezgif.com-optimize+%2843%29.gif)
![A COVID-19 Patient with 3 days of Symptoms [2/3]](https://images.squarespace-cdn.com/content/v1/58118909e3df282037abfad7/1584923302390-3HOKDDGEEXWXTE1ZKHPK/ezgif.com-optimize+%2844%29.gif)
![A COVID-19 Patient with 3 days of Symptoms [3/3]](https://images.squarespace-cdn.com/content/v1/58118909e3df282037abfad7/1584923302992-4BOINIWQM3AMUCPWU745/ezgif.com-optimize+%2845%29.gif)
![Hospitalized COVID-19+ Patient on Day 9 of Symptoms [1/2]](https://images.squarespace-cdn.com/content/v1/58118909e3df282037abfad7/1585424289744-RG5K8531BSVL0L2IF4NT/ezgif.com-optimize+%2848%29.gif)
![Hospitalized COVID-19+ Patient on Day 9 of Symptoms [2/2]](https://images.squarespace-cdn.com/content/v1/58118909e3df282037abfad7/1585424468095-8K5EKTWKAPOC1EYA9OAN/ezgif.com-optimize+%2849%29.gif)