Bowel-GI

Malignant Ascites
Malignant ascites with plankton sign in woman with metastatic ovarian cancer.
Samuel Eglin, MD
"Ring of Fire Sign" in Appendicitis
A 24 year old male comes to ER with abdominal pain, vomiting, and fever.
A directed scan with a high-frequency linear transducer in the right iliac fossa shows a tubular, non-compressible structure, a "target like" image, with increased echogenicity of the fat around it. When applied Color Doppler - we can observe increased vascular flow around the appendix - a sign known as "The Ring of Fire". This finding suggests the diagnosis of acute appendicitis.
Contributor: Renato Tambelli (@R_Tambelli @Jedipocus)

Taenia Saginata
Fatigue for the past 3–4 months with mild disturbance of bowel habits. The patient reported visualizing proglottids in the stool.
POCUS findings: Ultrasound performed in the left lower quadrant revealed a structure consistent with parasitic segments.
Diagnosis: Laboratory confirmation a few days later identified Taenia saginata.
Dr. Guillaume Schramme
To & Fro Peristalsis in Bowel Obstruction
Fecal material can be seen moving forward and backwards through dilated bowels in the patient with a bowel obstruction.
Contributed by: Brittany Garza, DO and Saleem Nasseh, MD and Sadie Ellenson, MS4

Free Fluid at Liver Tip
Free fluid demonstrated at the liver tip in a patient with ascites.
The liver tip is the most sensitive part of the RUQ for free fluid. In the context of blunt trauma this would be concerning for bleeding.
Contributors: Dimitri Livshits, DO; Jane Belyavskaya, MD; Chris Hanuscin, MD
Kings County/SUNY Downstate
Obstrução de Delgado - To and Fro sign
Sign of small bowel obstruction. We see heterogeneous material inside the loop of bowel with a back and forth movement, characterizing the obstruction. The patient in question had a paralytic ileus due to chronic antipsychotic use.
Felipe Teles; Internal Medicine at Fortaleza General Hospital
@drfelipemoraisteles
Tanga Sign (SBO)
Dilated loops of small bowel with free fluid adjacent to them (Tanga sign), CT confirmed SBO.
Dimitri Livshits DO, Ultrasound Fellow; Jane Belyavskaya MD, Ultrasound Fellow; Chris Hanuscin MD, Ultrasound Division Director (Kings County/SUNY Downstate)

To-and-Fro Peristalsis
Back and forth "to-and-fro" peristalsis consistent with SBO.
Dimitri Livshits DO, Ultrasound Fellow; Jane Belyavskaya MD, Ultrasound Fellow; Chris Hanuscin MD, Ultrasound Division Director (Kings County/SUNY Downstate)
Ascites in Pregnancy
22 year old G3P2 female presented to the ER, 18 weeks pregnant, with central abdominal pain with radiation to her back. She was found to have large volume ascites of unknown etiology on US. She was admitted to the hospital and underwent paracentesis. A reminder to keep a broad differential for abdominal pain, even if the patient is pregnant.
Michael Cannova, DO; Mara McMurray, DO
Acute Diverticulitis
60 year old man presenting with left lower quadrant pain and fever.
POCUS was performed and revealed a thick-walled colon and associated diverticula with surrounding hyperechoic fat stranding. Inside the pouch there's an echogenic structure casting deep shadowing consistent with a fecalith.
Alessandro Lena
Inguinal Hernia with Bowel and Bladder Involvement
This patient presented with acute onset, severe groin pain. On physical exam, a large inguinal hernia was appreciated, and the scrotum was enlarged, erythematous, and exquisitely tender to palpation. POCUS exam was performed and there were multiple bowel loops with active peristalsis and a large anechoic fluid collection. CT imaging confirmed this fluid to be a herniated portion of the bladder, which likely provided a good acoustic window for clear visualisation of the bowel loops.
Catherine Barrington MD, MSc, PGY1 Emergency Medicine, CMU; Andrew Namespetra MB BCh BAO, MSc, PGY3 Emergency Medicine, CMU
SBO Demonstrating To-and-Fro Peristalsis
Middle age male patient with past history of multiple abdominal surgeries, presented with clinical picture of intestinal obstruction. POCUS was performed demonstrating dilated bowel loops up to 3.3 cm with clear "to-and-fro" movements of bowel contents on the right side of the screen.
Learning point: Keep the ultrasound probe still and wait for enough time to allow the back and forth "to-and-fro" movements of the bowel content.
Contributor: Basel Elmegabar; MBBS

Ascites With Spider Web Sign
A 19 year old male, with hx of cocaine abuse presented to the ICU for respiratory insufficiency due to cardiogenic pulmonary edema. POCUS evaluation of the abdomen demonstrated ascites with Spider Web Sign, which is not expected in cardiogenic ascites. Because of this, peritoneal tuberculosis was suspected. It was later discovered that the patient had close contact with a person who was being treated for a confirmed tuberculosis diagnosis.
Contributor: Dr. Alessandro Ferreira
Hospital Metropolitano de Alagoas
Complicated Small Bowel Obstruction
This patient presented with a painful abdomen with distention and absent bowel sounds. Key findings in this scan include ineffective peristalsis as well as colon diameter that exceed 2.5 cm. Anechoic regions suggest presence of fluid which raise concern for a complicated small bowel obstruction.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Necrotizing Pancreatitis
In this case an elderly patient presented with severe back pain and an ultrasound exam was performed to evaluate the aorta. Instead in this transverse view, the pancreas was identified which appears enlarged with surrounding fluid. Besides appearing enlarged, an important finding in this scan is the hypoechoic regions which are indicative of necrosis.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Strangulated Hernia With Bowel Necrosis
This patient presented with a known paraumbilical hernia however what should be noted here are is the lack of peristalsis as well as the presence of air in the within the wall of the bowel. These findings suggest that necrosis has resulted from strangulation of a hernia. Other findings with this diagnosis that could also be found include hyperechoic fat, fluid within the sac, thickening of the hernial sac, dilated bowel and edema within the walls.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Perforated Viscus
Patient presented with altered mental status, hypotension and a rigid abdomen. It was unclear at the time if this patient’s presentation was due to trauma. Right-upper quadrant ultrasound used to view for potential cause using the perihepatic window. Here we can see air within fluid and a hyperechoic peritoneal stripe, indicating a perforated viscus. In this case, due to a duodenal ulcer.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Full Stomach
This clip demonstrates a full stomach. Gastric contents with internal air signatures can be seen swirling around within the stomach.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
SBO
45M history of exploratory laparotomy presented with abdominal pain, nausea, vomiting and decreased flatus. US shows dilated loops of bowel measured at 3.99 cm with to and fro movement of contents in greater than 3 areas consistent with small bowel obstruction.
Rachel Shing, MD
Boston Medical Center
Normal Bowel Peristalsis
51 year old male presented with a chief complaint of abdominal pain for 3 days with nausea and vomiting.
The curvilinear probe was used to evaluate the aorta with an incidental finding (shown) of clear peristalsis of the bowel contents with hypoechoic and anechoic contents. In this segment it is clear there is no obstruction.
Lindsay Davis, DO, MPH, @Lindsadavis18
Lydia Mansour, DO
Emily Nagourney, MS4
Central Michigan University
To-And-Fro of SBO
84 yo F presenting with abdominal pain, nausea, vomiting, constipation and abdominal distension for 3-4 days. Bedside ED-performed POCUS show this findings: No compressible and distended small bowel loops (> 2,5 cm), "To-and-Fro" motion of intraluminal content, “valvulae conniventes” on the interior aspect of the bowel wall, which appears like black and white keys of a piano (Keyboard Sign). These ultrasound signs rule-in the diagnosis of Small Bowel Obstruction.
Renato Tambelli
@JediPocus @R_Tambelli
Colonic Perforation with Abscess
RUQ scan revealed an isoechoic region adjacent to the hepatic flexure indicative of an abscess formation secondary to a colonic perforation.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Liver Metastasis
Patient with history of colon cancer presented with right flank pain. RUQ scan revealed metastatic liver disease.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Paraesophageal Abscess
Patient presented with chest pain. A subxiphoid sweep revealed normal cardiac function with a neighboring anechoic structure confirmed as a paraesophageal abscess on CT.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Pediatric gastrostomy replacement
Pediatric gastrostomy replacement with injection of oral rehydration solution into gastric lumen.
Cailin Frank

Unsuccessful pediatric gastrostomy replacement
Pediatric gastrostomy replacement NOT in gastric lumen - not only do you not see the stomach wall between the gastrostomy bulb and abdominal wall, with injection of oral rehydration solution you see it outline the spleen tip (near end of clip).
Cailin Frank
Pneumoperitoneum
POCUS reveals air bubbles rising in a patient with a perforated bowel obstruction resulting in a pneumoperitoneum.
Pancreatic Duct Stones
RUQ evaluation of a patient with chronic pancreatitis revealed pancreatic stones visible as hyperechoic structures within the pancreatic duct.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Direct Inguinal Hernia
An elderly female presented to the emergency department with left groin pain that had been intermittent for 6 months. At time of initial evaluation, she noted a “bump” in the left groin. On examination with POCUS, the inguinal canal was evaluated and revealed a direct left inguinal hernia. As the patient performs a Valsalva maneuver, bowel is seen moving into the canal. Upon release of Valsalva, the bowel reduces spontaneously.
Daniel Coffey, Emergency Medicine PGY-2; Jocelyn Garcia MS-3
Central Michigan University College of Medicine
Intussusception
Here we can see an intussusception. Multiple layers and concentric rings, target configuration on cross-sectional imaging.
Evgeny Domanin
Small Bowel Obstruction
30-year-old presented with 2-day history of abdominal pain, abdominal distention, and vomiting. Pertinent PMH includes prior hemicolectomy due to Crohn's disease. Seen here is POCUS evidence of SBO.
Ahmad Khan
@kadiwls
SBO
Small bowel obstruction (SBO) featuring “to and fro” movement and tanga sign.
Francisco Norman
Mesenteric Vasculitis
Patient has a history of SLE with abdominal pain and distention. POCUS shows abdominal free fluid and bowel wall thickening. Ultimately after CT and further testing confirmed this as SLE-induced mesenteric vasculitis.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Large Volume Ascites on Transverse Pelvic View
A 64-year-old woman with hepatic cirrhosis presented to the emergency room with abdominal pain. An abdominal POCUS exam was performed showing significant ascites. In this transverse pelvic view one can appreciate the uterus floating in ascites. This image finding is also known as the "TIE Fighter Sign" in reference to the famous Starwars galactic empire ship.
Image Courtesy of Dr. Renato Tambelli
SBO with "To-and-Fro"
A 58-year-old female with multiple prior abdominal surgeries presented with a 2-day hx of abdominal pain and N/V. ROS also notable for anorexia and constipation.
Abdominal POCUS seen here revealed dilated bowel loops with thickened and hyperechoic bowel walls. “To-and-fro” movements of the bowel contents are also appreciated. This occurs as a consequence of increased intestinal contents and peristalsis, otherwise known as dysfunctional peristalsis. All of the aforementioned are consistent with a diagnosis of SBO.
When there is high clinical suspicion of SBO, POCUS can serve as an inexpensive and rapid adjunct for clinical evaluation, expediting time to disposition.
Dr. Samantha Wong, @esayemDO
EM Resident. Central Michigan University
Small Bowel Obstruction
Small bowel obstruction showing a transition point in the ileum.
Steven Johnson
@alittlecoldgel
Pancreatic Pseudocyst
An elderly male with abdominal pain, hypotension and a palpable abdominal mass. POCUS revealed a normal sized pulsatile aorta with a large pancreatic pseudocyst.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Intra-abdominal Abscess
A middle aged female with a history of Crohns disease presented to the ED with fever, hypotension, and abdominal pain. Bedside ultrasound revealed an intra-abdominal abscess in the RUQ.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Ruptured Appendicitis with Intraabdominal Free Fluid
A 3 year old M presented with 3 days of fever, vomiting and abdominal pain. He was lethargic on arrival and found to be septic. POCUS shows ruptured appendicitis with a significant amount of hypoechoic fluid in the abdomen.
Paul Khalil, MD. Assistant PEM POCUS director at University of Louisville/Norton Children’s
@khalil3paul
Ruptured Appendix with Abscess Formation
A 2 year old F with 1 week of fever, vomiting, diarrhea and abdominal pain presented to the emergency department. A work up was initiated including POCUS of the right lower quadrant which revealed a ruptured appendix with abscess formation.
Paul Khalil, MD. Assistant PEM POCUS director at University of Louisville/Norton Children’s
Splenic Abscess
An elderly male with a history of IVDU presented to the ED with fever and abdominal pain. Vital signs reveal hypotension. RUSH examination revealed a splenic abscess viewed in the perisplenic window.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Mesenteric Adenitis
A young child presented to the ED with RLQ abdominal pain and a low-grade fever. Bedside ultrasound revealed enlarged, hypoechoic mesenteric lymph nodes with surrounding vascularity indicative of mesenteric adenitis. Be sure to rule out appendicitis.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Portal Venous Gas
An adult male presented to the ED with abdominal pain and hypotension. The perihepatic window of the RUSH exam reveals portal venous gas due to necrotizing pancreatitis. Also, note the trace free fluid in Morison’s pouch.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Pneumoperitoneum
Patient presented with severe right upper quadrant abdominal pain. POCUS revealed pneumoperitoneum due to a perforated duodenum. The pneumoperitoneum can be identified as the A-line pattern seen superior to a portion of the liver consistent with air in the wrong place!
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
To & Fro in Bowel Obstruction
This 70-year-old male presented to our ED reporting abdominal pain and vomiting with associated absence of flatus / bowel movements. Seen here is his LUQ abdominal view using the curvilinear probe that reveals a dilated loop of bowel. The image is further characterized by increased peristalsis (the "To and Fro" sign) as well as the presence of free fluid adjacent to the dilated bowel loop in the shape of a triangle (known as the "Tanga Sign"). This case highlights how bedside ultrasound can be a powerful tool to enable prompt diagnosis and treatment of bowel obstruction.
Renato Tambelli, Emergency Physician Hospital das Clínicas de Marília, Brazil.
@R_Tambelli // @JediPocus
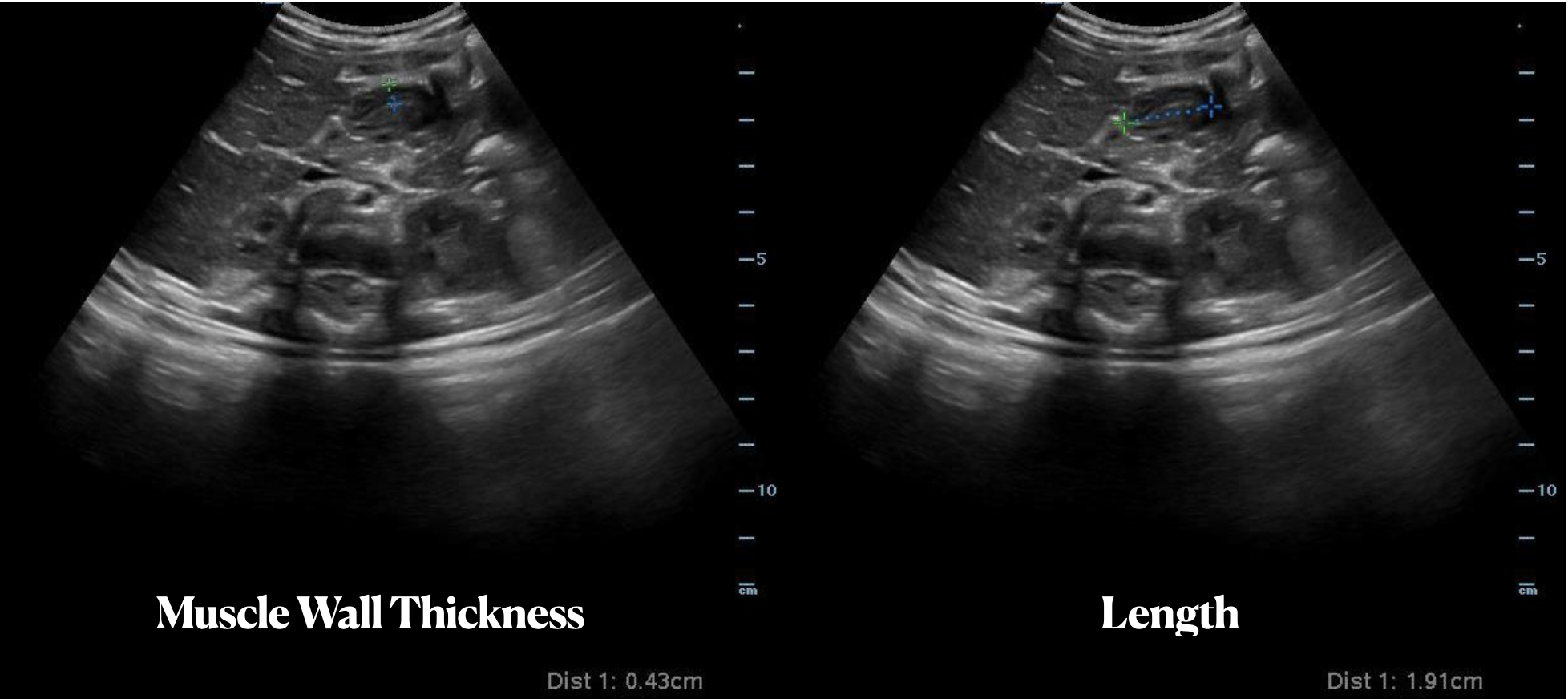
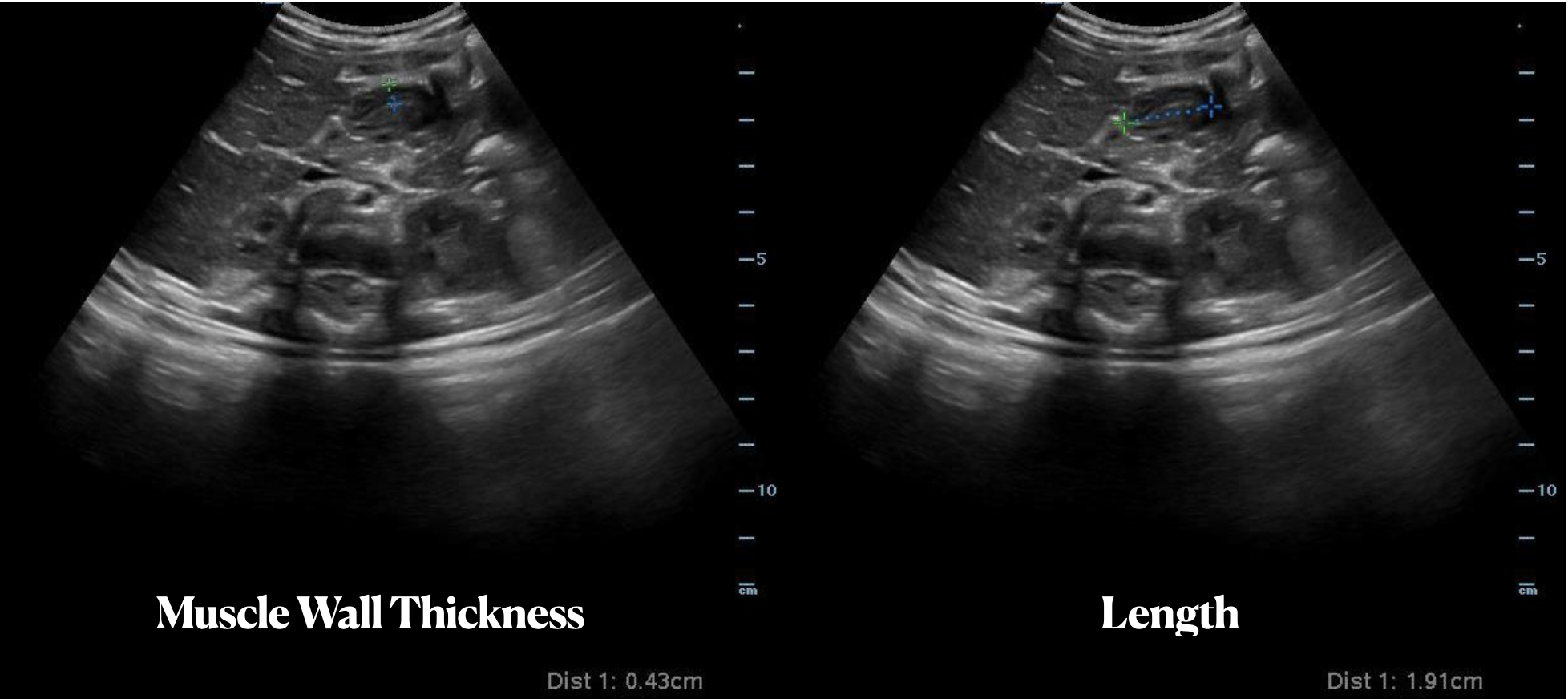
Measurements in Pyloric Stenosis
A 5 week old female previously healthy presents with 1 day of projectile vomiting. A bedside ultrasound was performed demonstrating muscle wall thickness of 4.3 mm (> 3 mm is abnormal) and a length of length of 19 mm (abnormal is >15 mm) consistent with a diagnosis of hypertrophic pyloric stenosis.
Paul Khalil, MD @Khalil3Paul
Assistant PEM POCUS Director at University of Louisville/Norton Children’s
Gallstone Ileus
An elderly male presented with unyielding bilious vomiting and abdominal pain. A RUQ extended view shows gallstone ileus with the hypoechoic stone creating an acoustic shadowing artifact. Here, the gallstone is lodged in the small bowel and can arise from frequent cholecystitis creating a fistula between the gallbladder and small bowel.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Hepatic hydrothorax
A 54-year-old male with hx chronic, untreated HCV complicated by cirrhosis presented with subacute dyspnea and abdominal distention. POCUS was notable for both a pleural effusion (anechoic fluid with atelectatic lung floating within it) as well as ascites (anechoic fluid underneath the mobile diaphragm). This history and POCUS findings were consistent with his diagnosis of hepatic hydrothorax.
Shahad Al Chalaby, MD. PGY-2, Internal Medicine
Highland Hospital. Alameda Health System Internal Medicine Residency Program. CA, USA
@shahad_Chalaby
Ascites with Pneumoperitoneum
Pt with PMH of cirrhosis presents with abdominal pain and fever. POCUS initially performed for diagnostic paracentesis in the setting of suspected spontaneous bacterial peritonitis. Imaging demonstrated bubbles seen in ascites fluid consistent with pneumoperitoneum. This led to management change as paracentesis was deferred and surgery was consulted. The patient was taken to the OR, and found to have a diverticular abscess with a necrotic segment that was resected.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Peritoneal Catheter Complication
Pictured here is a the proximal cuff of an indwelling peritoneal catheter. Note the abscess surrounding the cuff.
Javier Estrada, Nephrologist, Costa Rica
Ascites
70-year-old man with a history of alcoholic liver cirrhosis. Using a curvilinear probe on the left lower quadrant we appreciate significant ascites; also note the clear outline of bowel loops floating within the free abdominal fluid.
Renato Tambelli, Emergency Physician Hospital das Clínicas de Marília.Public Healthcare. Emergency Management.
@R_Tambelli
Pneumoperitoneum with Enhanced Peritoneal Stripe Sign
Pictured is a transversal epigastric abdominal view, first in M mode and subsequently B mode. Both modes reveal Enhanced Peritoneal Stripe Sign (EPSS), a finding that is highly sensitive and specific for pneumoperitoneum. An A-line pattern is also appreciated in this clip, due to reverberation artifact caused by the free air. This pattern mimics the A-line pattern seen in normal lung tissue.
We were able to make this diagnosis with a portable POCUS device in the Emergency Department!
Renato Tambelli, Emergency Physician
@R_Tambelli
Fibrinous Ascites
A patient with cirrhosis presented with severe abdominal pain. POCUS of the abdomen revealed significant anechoic ascites. The quality of the ascites is also notable for presence of fibrinous material, increasing the pre-test probability of SBP.
Paracentesis confirmed presence of >6000 WBCs; though this unique POCUS finding enabled earlier initiation of antimicrobial therapy for this patient.
Parker Dixon, Hospitalist
@drparkerdixon
The Keyboard Sign
A patient presented to the emergency department with one day of constipation and abdominal distention.
A bedside ultrasound was performed showing dilated bowel, to-and-fro peristalsis, and keyboard sign (plicae circulares). Low-grade SBO with transition point found on follow up CT.
Aaron Inouye
@PAintheED
Perisplenic Hematoma
This clip is from a patient presenting with sudden onset epigastric pain with syncope. The patient had an additional episode of syncope in the ED and remained persistently hypotensive. The aorta was evaluated and was non-aneurysmal, however during FAST exam the LUQ view demonstrated a perisplenic hematoma and free fluid was also noted in Morrison’s pouch (RUQ view not shown). CT of the abdomen/pelvis later confirmed spontaneous splenic rupture.
Nishant Cherian
Fluid Filled Periumbilical Hernia
27 year old male with a history of cirrhosis presenting with increased swelling of the periumbilical area. A bedside ultrasound was performed demonstrating a fluid filled hernia sac from the patient’s known ascites.
Mario Corro, MD, PGY-3 & Josh Greenstein, MD
Staten Island University Hospital
Complex Ascites
A 70 year old male with history of pancreatic cancer presented with abdominal distention. POC US demonstrated complex ascites. As seen in this clip, complex ascites (such as from malignancy) often demonstrates loculations as well as layering due to dense particulate (exudative ascites) within the fluid.
Mario Corro, MD, PGY-3 Staten Island University Hospital
Acute Appendicitis with Appendicolith
This image is from a patient presenting with right lower quadrant pain. It demonstrates findings of acute appendicitis including : a dilated fluid filled structure with thickened walls, surrounding hyperechoic fat (fat stranding) and an appendicolith.
Check out our colorized image post on evaluating for acute appendicitis here.
Image Courtesy of IUEM Ultrasound
Original Twitter Post can be found here.
Strangulated Inguinal Hernia
60 year old male presents with pelvic and scrotal pain with vomiting x 1 hour. Physical exam significant for an edematous, erythematous, tender scrotum. Bedside ultrasonography revealed bowel peristalsis and marked scrotal edema (anechoic stripe) visible throughout the scrotum with several loops of bowel within the scrotum. IV established for analgesia and nausea control, and general surgery was consulted. The surgeon requested a CT even though there was good certainty of a strangulated hernia, for operative planning purposes. Patient went to the OR the same day and made full recovery.
Pieter Ver Steeg, PA-C
Inguinal Hernia With Peristalsis
33 y/o M p/w LLQ and groin pain since bending and lifting heavy boxes the day before. Clinically appears to have an inguinal hernia. Using the inguinal ligament as a guide, the inguinal canal is found at the midpoint between the ASIS and pubic symphysis, just superior to the ligament. The epigastric vessels mark the deep opening of the canal. This can help determine an indirect from direct inguinal hernia. It is estimated that the sensitivity and specificity of POCUS for inguinal hernia detection are 97% and 87% respectively. PMID: 12831490
This is a transverse cut across the left inguinal canal. As the probe moves downward toward the left scrotum, you can see a small loop of bowel contained within the canal. To confirm this is bowel, peristalsis can be seen with fecal material moving in the lumen. There does not appear to be hyperemia or free fluid indicating incarceration or strangulation. The patient was referred to general surgery for repair.
Ronald J. Rivera, PGY3
SUNY Downstate / Kings County Emergency Medicine
This is the article I used for the sensitivity and specificity:
Gastric Feeding Tube
Control of gastric feeding tube.
Case of gastric tube placed in the stomach. You might consider the use of color doppler to see flow pattern in the lumen.
Dr. Birkelund
Small Bowel Obstruction
A 60 female presented with 3 days of vomiting, suprapubic distension and left groin pain. POCUS shows distended bowel loops (>2.5cm), 'to-and-fro' motion of hyperechoic bowel contents and extraluminal free fluid. NG was passed for decompression and surgical admission arranged. CT showed small bowel obstruction at the level of distal ileum within a left inguinal hernia
Dr Cian McDermott, Mater University Hospital, Dublin, Ireland
Small Bowel Obstruction
Visualized here are dilated loops of bowel as a result of SBO. One can see hyperechoic fecal material moving to and fro due to blocked peristalsis, visible plicae circularis (folds of small bowel mucus membrane that increase surface area for absorption) also known as the "piano sign," and abdominal free fluid between loops known as "tanga sign."
Sukh Singh, MD
Small Bowel Obstruction
65 female patient 6 months post bowel resection (lower midline laparotomy scar) presents with vague abdominal pain. She is maximally tender over the scar. Bedside ultrasound shows dilated bowel loops and 'to and fro' peristaltic movements. CT confirmed small bowel obstruction and her care was expedited
Dr Cian McDermott, Mater University Hospital, Dublin, Ireland
Incarcerated Hernia with SBO
29 yo F with known hernia p/w sudden onset abdominal pain 2hrs ago. Given a concern for an incarcerated hernia, POCUS was done showing the incarcerated loop of bowel (hypoechoic structure on the left), as well as evidence of an SBO. In addition to a dilated loop (+LR of 15 for 3 loops >2.5cm), the hyperechoic lines along the bowel represent valvulae conniventes which are suggestive of an obstructed loop of jejunum. Patient happened to be pregnant (17wks, FHR and motion also confirmed by POCUS), but was taken emergently to the OR for open repair with mesh and was discharged the next day.
Bryan Jarrett, MD - SUNY Downstate/Kings County
Small Bowel Obstruction
These images were recorded from an elderly lady with abdominal pain and vomiting. Small bowel lumen is dilated more than 2.5cm and there is reduced peristalsis within the lumen - these sonographic signs are consistent with small bowel obstruction (SBO). Other signs of SBO include the presence of hyperechoic material moving back and forth within the bowel lumen and free fluid between the loops of bowel (Tanga sign).
Images by Dr. Rory Whelan
Submitted by Dr. Cian McDermott - Dublin, Ireland
Iguapoo Falls
Small bowel obstruction with a steep precipice and tumbling feces. We call this Iguapoo falls.
Andrew Liteplo MD, RDMS - Massachusetts General Hospital
Chief, Division of Ultrasound in Emergency Medicine
Director, Emergency Ultrasound Fellowship
Small Bowel Obstruction
67 y/o M with PMH colon cancer s/p resection and colostomy, multiple SBO managed conservatively p/w no colostomy output for 3 days and increasing abdominal distention.
POCUS shows fluid-filled, noncompressible small bowel loops dilated >2.5 cm, the most sensitive finding for POCUS diagnosis of SBO. You also see characteristic to-and-fro motion of the bowel contents. You do not see signs of severe obstruction such as extraluminal free fluid, no peristalsis, or bowel wall thickening >3 mm. Recent studies report a very high positive likelihood ratio for POCUS: 9.55 for clinical US, compared to 1.6 for radiographs, 3.6 for CT, and 6.8 for MRI. Now just convince your surgeons...
Dr. Angela Cai, Dr. Kelly Maurelus - Kings County/SUNY Downstate Emergency Medicine
https://www.acep.org/Content.aspx?id=100218#sm.0001bhfy70l03elmtz51w5hlmrnna
Duodeno-Biliary Fistula
Tiny bubbles of air float up to the top of the gallbladder. This finding prompted additional work-up and an ultimate diagnosis of duodeno-biliary fistula.
Rachel Haney, MD - Massachusetts General Hospital
Ascites... hello?
WCUME17 submission: "Creative Caption"
"Well hellllllo there...I'm so ASCITED to see you!"
Patient with ascites and a surprising greeting on POCUS.
Dr. Stephen Alerhand - Mount Sinai Hospital
Small Bowel Obstruction
This image demonstrates a dilated loop of small bowel with to and fro movements of stool contents. POCUS has been shown to have a sensitivity of 0.91 and specificity of 0.84 for this indication in a single trial when EM residents performed the study. This is compared to 0.02 and 0.67 for an old fashioned KUB.
Jang TB, et al. Bedside ultrasonography for the detection of small bowel obstruction in the emergency department. J Emerg Med. 2011. 28(8):676-678.
Submitted by Dr. Justin Bowra et al.
Gastric Volvulus
80 y/o demented M patient comes in with complaint of abdominal distention, noticed by caregivers. Patient "not keeping anything down." POCUS was done to visualize the "distention."
Fluid is seen in what was presumably the stomach, moving forward and backward, not passing the pylorus. The distal bowel did not contain similar fluid. CT demonstrated gastric volvulus and GI was consulted.
Dr. Bryan Jarrett - Kings County/SUNY Downstate Emergency Medicine
Biliary Colic That Wasn't
This is an image from a 55 years gentleman with suspected biliary colic. A gallstone was confirmed however the patient's symptoms during exam did not match classic biliary colic. A more in depth evaluation of the right upper quadrant confirmed the presence of a right colonic mass. Color flow was appreciated on a separate clip. Although bowel pathologies are an uncommon finding with emergency ultrasound, they can be easily found with further investigation in atypical presentations.
Stefanie Tamburrini, MD
Emergency Radiologist
Reducing Aspiration Risk
A 76 y/o F ward patient was vomiting and in respiratory distress possibly due to aspiration. The patient had impending respiratory failure and the plan was to intubate and admit to ICU. A POCUS was done to evaluate her distended abdomen prior to intubation and the image demonstrated a grossly distended stomach with swirling hyperechoic particles. NG tube was placed and approximately 1 liter of bilious fluid was removed. Patient was safely intubated thereafter with aspiration risk minimized.
Learning point: For peri-intubation patient with high aspiration risk, POCUS can help determine the amount of gastric content and potentially alter management to include maneuvers to minimize aspiration risk.
Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014 Jul;113(1):12-22. doi: 10.1093/bja/aeu151.
Submitted by Leon Chen, NP – Critical Care Medicine Service
Department of Anesthesiology and Critical Care Medicine
Memorial Sloan Kettering Cancer Center - New York, NY
Intussusception Adult
Intussusception is typically a disease of the young (6 months to 6 years) but it can occur in adults. Adults will often present similar to bowel obstruction, with vomiting, constipation, and rectal bleeding. Ultrasound can still be used to work them up although most of the time CT will be used first.
In kids, the sensitivity and specificity approach 100% but can be operator dependent. It is usually performed with a linear probe in children but in this image, a curvilinear probe was used.
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al.
Enlarged Appendix with Appendicolith
This images demonstrates a longitudinal view of an appendix that appears enlarged with edematous walls, containing a shadowing appendicolith, consistent with acute appendicitis.
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al.
The Piano Sign
A 55 year old male came to ED c/o abdomen pain for 3 days associated with abdominal distention and vomiting. He was noted to be tachycardic and his abdominal exam demonstrated tenderness and bulging in the right inguinal area.
A curvilinear probe was used to evaluate for bowel obstruction. The clip demonstrates a dilated loop of bowel, "to and fro" movements of bowel content suggesting dysfunctional peristalsis, and the piano sign. The piano sign (or keyboard sign) is essentially visualization of the plicae circularis which is associated with the diagnosis of small bowel obstruction.
Dr. Mahmoud S Alsomali
EM Resident R4; Saudi Board Of Emergency Medicine; King Saud Medical City; Riyadh KSA
Perforated Appendicitis
30 y/o F with chills, constipation for 3 days. Normal labs and vitals, but distinctly tender in the RLQ. POCUS revealed free fluid and surrounding bowel wall edema with a structure floating that is likely the appendix.
CT confirms a perforated appendix with trace free air complex fluid and thickening of the adjacent bowel wall.
Dr’s Sophia Sharifali, Esther Kwak, and John F Kilpatrick -
Kings County/SUNY Downstate Emergency Medicine
Bowel Gas
Bowel gas scatters ultrasound waves making the structure containing the gas as well as posterior structures difficult to visualize. Applying more gentle graded pressure to the probe may displace the gas and improve visualization.
Sukh Singh, MD
Retrocecal Appendicitis
A non-compressible appendix with appendicolith is seen with surrounding fat stranding posterior to a decompressed cecum.
Sukh Singh, MD
Enlarged pylorus with gastric outlet obstruction
28 y/o F no significant PMH with 1 month epigastric abdominal pain associated with daily emesis in the mornings and postprandial discomfort.. Patient notes she feels a firmness in her epigastrium. POCUS with an enlarged pylorus with gastric outlet obstruction, confirmed with formal sono. Admitted and evaluated with EGD by GI, found to have peptic ulcer in the antrum with edema and degree of gastric outlet obstruction.
Dr. Adrian Aurrecoechea, Dr. Andrew Aherne - Kings County Hospital
Free fluid and Collapsed Bowel
23 year old male with no known medical history s/p surgery for sigmoid volvulus presenting with severe lower mid-abdominal pain. Ultrasound showed trace free fluid and significant collapsed bowel with no peristalsis. CT scan findings were equivocal to our US findings. Patient was found to have bowel dehiscence in the operating room.
Bowel wall is most easily seen when there is free fluid or ascites. Normal bowel has layered appearance, easily compressible with intermittent peristalsis. The most frequent pathological findings found by ultrasound is wall thickening, mucosal abnormalities, the absence of peristalsis (1). One benefit of point-of-care intestinal ultrasound is decision for early surgery. Sonographic findings suggesting a need for surgery include; intraperitoneal free fluid, bowel wall thickness of more than 4 mm, and decreased or absent peristalsis (2).
Valette PJ, Rioux M, Pilleul F, Saurin JC, Fouque P, Henry L, Eur Radiol. 2001; 11(10):1859-66.
Grassi R, Romano S, D'Amario F, Giorgio Rossi A, Romano L, Pinto F, Di Mizio R, The relevance of free fluid between intestinal loops detected by sonography in the clinical assessment of small bowel obstruction in adults. Eur J Radiol. 2004 Apr; 50(1):5-14.
Dr Catharine Bon and Dr Bobak Zonnoor Kings County Emergency medicine
Free Fluid and Collapsed Bowel
23 year old male with no known medical history s/p surgery for sigmoid volvulus presenting with severe lower mid-abdominal pain. Ultrasound showed trace free fluid and significant collapsed bowel with no peristalsis. CT scan findings were equivocal to our US findings. Patient was found to have bowel dehiscence in the operating room.
Bowel wall is most easily seen when there is free fluid or ascites. Normal bowel has layered appearance, easily compressible with intermittent peristalsis. The most frequent pathological findings found by ultrasound is wall thickening, mucosal abnormalities, the absence of peristalsis (1). One benefit of point-of-care intestinal ultrasound is decision for early surgery. Sonographic findings suggesting a need for surgery include; intraperitoneal free fluid, bowel wall thickness of more than 4 mm, and decreased or absent peristalsis (2).
Valette PJ, Rioux M, Pilleul F, Saurin JC, Fouque P, Henry L, Eur Radiol. 2001; 11(10):1859-66.
Grassi R, Romano S, D'Amario F, Giorgio Rossi A, Romano L, Pinto F, Di Mizio R, The relevance of free fluid between intestinal loops detected by sonography in the clinical assessment of small bowel obstruction in adults. Eur J Radiol. 2004 Apr; 50(1):5-14.
Dr Catharine Bon and Dr Bobak Zonnoor Kings County Emergency medicine
Esophagus Swallowing
In the center of the screen we see the trachea in transverse view with its round hyperechoic cartilaginous rings. To the right of the trachea is the smaller, collapsed, muscular walled esophagus which moves as the patient swallows in this clip. We can also see the pulsatile carotid arteries bilaterally at the edges of the screen.
Duodenum
In this clip the probe is positioned over the RUQ. The liver is on the left side of the screen, and in the center of the screen we see a portion of the duodenum in cross-section. Often mistaken for a gallbladder full of gallstones by novices sonographers, it can be identified by its peristaltic waves with visible motion of the bowel contents within.
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Large Bowel
This clip shows a segment of the colon in long axis beneath layers of connective tissue and muscle. The peristalsis of the bowel is clearly visible as demonstrated by the motion of its inner contents.
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Appendicitis Transverse
30 y/o M w/ subjective fever, RLQ pain x1day. Tenderness in McBurney’s point w/positive Rovsing’s and Psoas signs, labs significant for mild leukocytosis.
POCUS w/ linear probe placed on area of maximal tenderness in RLQ. Transverse and longitudinal views demonstrated non-compressible, blind-ended, non-peristalsing, tubular structure with surrounding hypoechoic free fluid. A central hyperechoic structure representing a fecalith can be appreciated. Outer diameter was measured to be 10mm representing dilated appendix. Findings of acute appendicitis were confirmed with official ultrasound and pt was taken to OR for appendectomy without CT (limiting radiation for young adult). While POCUS is operator dependent and CT is gold-standard for diagnosis of appendicitis in adults, our POCUS findings had higher positive-predictive value given high pre-test probability (classic sx of appendicitis, alternate diagnoses less likely) and optimal pt for study (thin male, no prior surgeries).
Dr. Robert Allen and Dr. Matthew Riscinti - Kings County Emergency Medicine
Appendicitis Longitudinal
30 y/o M w/ subjective fever, RLQ pain x1day. Tenderness in McBurney’s point w/positive Rovsing’s and Psoas signs, labs significant for mild leukocytosis.
POCUS w/ linear probe placed on area of maximal tenderness in RLQ. Transverse and longitudinal views demonstrated non-compressible, blind-ended, non-peristalsing, tubular structure with surrounding hypoechoic free fluid. A central hyperechoic structure representing a fecalith can be appreciated. Outer diameter was measured to be 10mm representing dilated appendix. Findings of acute appendicitis were confirmed with official ultrasound and pt was taken to OR for appendectomy without CT (limiting radiation for young adult). While POCUS is operator dependent and CT is gold-standard for diagnosis of appendicitis in adults, our POCUS findings had higher positive-predictive value given high pre-test probability (classic sx of appendicitis, alternate diagnoses less likely) and optimal pt for study (thin male, no prior surgeries).
Dr. Robert Allen and Dr. Matthew Riscinti - Kings County Emergency Medicine
GI Tumor - GIST
Gastrointestinal Stromal Tumor (GIST)
58 y/o F no PMH with epigastric pain for two days, nausea and generalized weakness but no other symptoms. Vital signs were normal and physical exam was limited due to obesity but revealed moderate tenderness in the epigastric region without distention or peritoneal signs. The remainder of the exam was unremarkable and POCUS was performed.
A subcostal view is above showing an undefined hypoechoic, heterogeneous, cystic mass. It was non-compressible with well defined borders.
Computed tomography (CT) of the abdomen and pelvis confirmed a large, heterogeneous mass adjacent to the stomach with a small amount of intra-abdominal and intra-pelvic blood. The patient was admitted to general surgery, and endoscopic ultrasonography with biopsy revealed a spindle cell lesion consistent with gastrointestinal stromal tumor (GIST).
Gastrointestinal stromal tumors are the most common mesenchymal tumors of the GI tract with an incidence of 14 to 20 cases per million.(1) They can be located anywhere in the GI tract but are most frequently identified in the stomach (50-60%) and small bowel (30-40%).(2) Symptoms include abdominal pain, nausea, dyspepsia, fatigue, constipation, or diarrhea. Gastrointestinal stromal tumors have varying appearance on different imaging modalities and are often first seen on abdominal ultrasonography.(3)
A subcostal view is be a good place to begin POCUS, considering that most GISTs are located adjacent to or within the stomach. Case reports describe the diagnosis of GIST with help of initial transabdominal ultrasonography.(4,5) Appearance on ultrasonography may vary, depending on size and mitotic activity.(3) Larger tumors may often appear as heterogeneous masses, filling the abdomen with hypoechoic areas consistent with necrosis.(1) However, reports also describe tumors initially seen as extraluminal hypoechoic masses of varying size.(5)
While transabdominal ultrasonography is an excellent starting point, CT ultimately shows better detail for staging and characterization. Endoscopic ultrasonography can be used for further definition and ultimately for diagnosis, as biopsy is required.
Point-of-care ultrasonography may be an excellent tool for determining further management of patients with non-specific abdominal symptoms. While you may not initially suspect a GIST when starting your POCUS, an unidentifiable mass in the GI tract should prompt further investigation, which can ultimately lead to formal diagnosis.
References
Vernuccio F, Taibbi A, Piccone D, et al. Imaging of Gastrointestinal Stromal Tumors: From Diagnosis to Evaluation of Therapeutic Response. Anticancer Research 2016;36(6):2639–48.
Wronski M, Cebulski W, Slodkowski M, Krasnodebski I. Gastrointestinal Stromal Tumors . Journal of Ultrasound 2009;28(7):941–8.
King DM. The radiology of gastrointestinal stromal tumours (GIST). Cancer Imaging 2005;5(1):150–6.
Sugihara T, Koda M, Tanimura T, Yoshida M, Muruwaki Y. A report of three cases of exophytic gastrointestinal stromal tumor detected by transabdominal ultrasound. Journal of Medical Ultrasonics 2016;43(1):107–11.
Chan KP. What’s the Mass? The Gist of Point-of-care Ultrasound in Gastrointestinal Stromal Tumors. Clinical Cases and Reports in EM 2018;2(1).
SBO
60 y/o M hx CHF, ventral hernia s/p repair p/w abdominal pain, nausea, vomiting without flatus. POCUS shows dilated fluid filled small bowel loops > 3 cm in size. There are signs of bowel wall edema with folds projecting into the lumen known as "piano sign" as well as alternating propulsive and retrograde movement of contents which is frequently described as "washing machine sign" typically seen in small bowel obstruction.
Jaramillo, Juliana MD; Shah, Rushabh MD; Aherne, Andrew MD; Cutright, Molly MD.
Cirrhosis
70-year-old man with a history of alcoholic liver cirrhosis. This RUQ view obtained with a curvilinear probe reveals a cirrhotic liver (reduced dimensions with irregular edges and an overall heterogenous echotexture) surrounded by significant ascites within Morison's Pouch.
Renato Tambelli, Emergency Physician Hospital das Clínicas de Marília.Public Healthcare
@R_Tambelli
Floating Liver
A 59 year old male with known history of alcoholic cirrhosis presented with dyspnea. Physical exam was notable for a distended, non-tender abdomen. POCUS performed on the RUQ using the curvilinear probe revealed the liver “floating” within ascites. This highlights the importance of performing POCUS to guide procedures, as the patient subsequently warranted therapeutic paracentesis.
Victor Bang, Emergency Clinician at Hospital das Clínicas de Marília. Co-Founder of Pocus Jedi
@vmjbang
Cholangiocarcinoma with Metastases
Cholangiocarcinoma with liver metastases and biliary sludge.
Sukh Singh, MD
Hepatic Cysts
Large hepatic cysts. They were large enough to cause hepatomegaly clinically.
Dr. Gordon Johnson
Hepatic Lesions (Incidental)
Incidental cystic and necrotic lesions seen throughout liver in a patient with hepatomegaly and abdominal pain on exam. Primary pancreatic CA (not shown). It is still difficult to have a poker face while finding surprise cancer with POCUS.
Jason Tanguay, DO
Whirlpool Sign
A 6-day-old presented with findings suggestive of volvulus. POCUS revealed whirlpool sign, consistent with midgut volvulus. The sign corresponds to a clockwise wrapping of the superior mesenteric vein and the mesentery around the superior mesenteric artery (augmented with color doppler in the image on the right).
Michael Cooper
Pediatric appendicitis
Pediatric appendicitis: 4mm appendicolith in mid-appendix with surrounding edema.
Aaron Inouye, PA-C
Emergency Medicine. North Canyon Medical Center, Idaho
@PAintheED
Appendicitis (Long Axis)
18 y/o with severe acute onset RLQ abdominal pain, associated with vomiting. Temp 100.8 with guarding over RLQ. POCUS performed and revealed appendicitis.
8mm dilated, non-compressible, aperistaltic appendix with an appendicolith present (hyperechoic structure in blind end of appendix) surrounded by free fluid. Tender directly over the appendix. The psoas muscle can be seen on the right side, and bowel can be seen to the left.
Drs. Bryan Jarret, Sathya Subramaniam - Kings County/SUNY Downstate
Appendicitis with two fecaliths
Patient with RLQ pain, ttp, fever and guarding. POCUS performed at area of maximal tenderness demonstrating a dilated appendix >6mm with a blind distal end and sonographic McBurney's. Two fecaliths can be visualized, one at the distal end and a smaller one more proximally (right side of the screen).
Dr. Sathya Subramaniam - Children's Hospital of Philadelphia
Appendicitis + Free Fluid
18 y/o with severe acute onset RLQ abdominal pain, associated with vomiting. Temp 100.8 with guarding over RLQ. POCUS performed and revealed appendicitis.
8mm dilated, non-compressible, aperistaltic appendix with an appendicolith present (hyperechoic structure in blind end of appendix) surrounded by free fluid. Tender directly over the appendix. The psoas muscle can be seen on the right side, and bowel can be seen to the left.
Drs. Bryan Jarret, Sathya Subramaniam - Kings County/SUNY Downstate
Normal Appendix (Longitudinal)
13 y/o F with several days of suprapubic pain, dysuria, nausea, vomiting, tender to palpation in the suprapubic and RLQ area. This study was eventually repeated and confirmed as normal.
The appendix was visualized on both longitudinal and transverse views as a blind-ended structure overlying the iliac vessels, a typical location for the appendix. In this view the slightly dilated blind end can be seen to the right of the screen as it tapers off to the left side of the screen. The pulsating iliac vessels can be seen below. This study was eventually repeated and confirmed as normal.
Dr. Sathya Subramaniam, Pediatric EM Fellow - Kings County/SUNY Downstate
Appendicitis
15 year old female with no PMH with 3 days of RLQ abdominal pain, nausea, vomiting with inability to tolerate PO, RLQ tenderness. Bedside POCUS performed for suspected appendicitis.
The psoas muscle and iliac vessels were used as landmarks and free fluid was identified. This prompted closer scanning through the fluid. When the probe was rotated to a sagittal plane, a tubular structure with blind end was identified surrounded by free fluid. CT later confirmed appendicitis and patient went to surgery.
Drs. Praneetha Chaganti, Kyle Kelson, Scott Kendall - Kings County/SUNY Downstate Emergency Medicine
Normal Appendix (Transverse)
13 y/o F with several days of suprapubic pain, dysuria, nausea, vomiting, tender to palpation in the suprapubic and RLQ area.
The appendix was visualized on both longitudinal and transverse views as a blind ended structure overlying the iliac vessels, a typical location for the appendix. In this view the iliac vessels and psoas muscle can clearly be visualized to the right of the appendix viewed in cross section. This study was eventually repeated and confirmed as normal.
Dr. Sathya Subramaniam, Pediatric EM Fellow - Kings County/SUNY Downstate
Normal Appendix - Cross Section Measured
12 y/o M with nausea vomiting fevers and vague “belly pain.” Patient mildly tender in suprapubic area. POCUS visualized a normal appendix is seen. A normal appendix is identified by a blind-ending tubular structure that is <6mm diameter measured from outer wall to outer wall (although 6mm-7mm has also been described). This patient’s appendix was measure to be 5.1mm.
Dr. Sathya Subramaniam - Children’s Hospital of Philadelphia
Appendicitis - Ring of Fire
12 y/o with appendicitis. Using color-flow doppler, you can see increased vascularity surrounding the appendix, referred to as a “Ring of Fire”
Dr. Sathya Subramaniam
Normal Appendix blind end
12 y/o M with nausea vomiting fevers and vague “belly pain.” Patient mildly tender in suprapubic area. POCUS visualized a normal appendix is seen. A normal appendix is identified by a blind-ending tubular structure (as seen in this image). It should be <6mm diameter measured from outer wall to outer wall (although 6mm-7mm has also been described). This patient’s appendix was measure to be 5.1mm (see still image).
Dr. Sathya Subramaniam - Children’s Hospital of Philadelphia
Normal Appendix - Cross Section
12 y/o M with nausea vomiting fevers and vague “belly pain.” Patient mildly tender in suprapubic area. POCUS visualized a normal appendix is seen. A normal appendix is identified by a blind-ending tubular structure that is <6mm diameter measured from outer wall to outer wall (although 6mm-7mm has also been described). This patient’s appendix was measure to be 5.1mm (see still image).
Dr. Sathya Subramaniam - Children’s Hospital of Philadelphia
Normal Appendix - Blind End
A normal appendix is identified by a blind-ending tubular structure (as seen in this image). It should be <6mm diameter measured from outer wall to outer wall (although 6mm-7mm has also been described). This patient’s appendix was measure to be 5.4mm (see still image).
Dr. Sathya Subramaniam - Children’s Hospital of Philadelphia
Retroperitoneal Hemorrhage
An elderly male presented to the ED with hypotension and abdominal pain. Ultrasound revealed retroperitoneal fluid in perirenal and anterior pararenal spaces.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Pelvic Free Fluid in Ruptured Appendicitis
Free fluid is noted in this clip from the pelvic region during a RUSH exam in a patient with a ruptured appendicitis.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Appendix - Colorized
Appendix
Red: Iliac vessels, Green: Appendix
Images: Dr. Lindsay Davis, Dr. Hannah Kopinski. Image Editing: Michael Amador and Dr. Matthew Riscinti
Large Bowel - Colorized
Large Bowel
Orange - Large bowel lumen
Images: Dr. Lindsay Davis, Dr. Hannah Kopinski. Image Editing: Michael Amador and Dr. Matthew Riscinti
Duodenum - Colorized
Duodenum and Liver
Orange: Duodenum, Red: Liver
Images: Dr. Lindsay Davis, Dr. Hannah Kopinski. Image Editing: Michael Amador and Dr. Matthew Riscinti
Portal Venous Gas From Diverticular Abscess
This is a clip demonstrating portal venous gas. Notice air can be seen as hyperechoic signals extending to the periphery of the liver. Air signal can also be seen within the flat IVC. Free intraperitoneal fluid is also present.
Patient was ultimately found to have a large diverticular abscess.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here

Small Bowel Obstruction
50s M with no surgical history presented with upper abdominal pain, biliary POCUS was performed which was negative, but large amounts of bowel gas were seen. Small bowel dilation was seen with multiple loops of bowel >2.5cm in diameter with bidirectional flow of bowel contents. CT confirmed SBO and the patient was taken to the OR for operative management
Spencer Seballos MD, Resident, Denver Health Residency in Emergency Medicine
Katie McCabe MD, Attending Physician, Denver Health Residency in Emergency Medicine