Left Ventricular Dysfunction
New Onset Cardiomyopathy with Reduced Ejection Fraction
47 year-old male with no cardiac history presenting with shortness of breath and leg swelling for two weeks found to have new onset cardiomyopathy. POCUS echocardiogram showed significant dilation of the LV on parasternal long axis view with reduced EF; EPSS of 23.7 mm. Formal echocardiogram confirmed findings with additional findings including EF <20%, mild dilation of the LA, RA, and RV. While LV is grossly dilated, the significantly increased EPSS correlates with the dramatically reduced EF.
Brent Oldham, MD, MPH, PGY-3, Central Michigan University College of Medicine, Emergency Medicine
Dan Dunaske, DO, PGY-1, Central Michigan University College of Medicine, Emergency Medicine
Brad Buska, MS4, Central Michigan University College of Medicine
Biventricular Failure
90 y/o F presents with hypotension. Patient was signed out to me by the overnight team with "sepsis" and received 30 cc/kg bolus. Patient began to have SBPs in the 70s again. She was immediately placed on vasopressors and managed for a CHF exacerbation. Image is a slightly obliqued PSAX.
John Bowling, DO, Cleveland Clinic Akron General, @BModeBowling
The image is slightly oblique giving the LV an oval appearance
Post COVID Myocarditis
A 29-year-old patient, with a recent history of mild COVID 19 infection, consulted for a 5-day history of fever, associated with abdominal pain, arthralgia and myalgia. Hypotensive on admission (80/50 mmHg), with HR 100 bpm and echocardiography performed with a convex transducer: LVEF 12%, with global hypokinesia and dilated cavities. The diagnosis of post-COVID myocarditis is made.
Dr. Libardo Valencia Chicué
Postpartum Cardiomyopathy
This healthy patient presented 3 months postpartum with progressive dyspnea over the past few weeks found to have new postpartum cardiomyopathy with EF about 10-15% as demonstrated in the parasternal long axis view.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here.
Takotsubo Cardiomyopathy on Apical Two Chamber View
Apical 2 chamber view showing akinesia of the apical walls characteristic of Takotsubo cardiomyopathy.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Reduced Ejection Fraction (Parasternal Long Axis View)
Patient with systolic heart failure with reduced ejection fraction.
Nigist Taddese MBChB
Division of Hospital Medicine, John H Stroger Hospital of Cook County
Ventricular Fibrillation
Subcostal view of a patient reentering ventricular fibrillation following ROSC.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Post Myocardial Infarction VSD
This patient presented with worsening “GERD” symptoms over the past 8 days, found to have markedly elevated troponin and anterior STEMI on ECG.
The parasternal long axis view revealed a ventricular septal defect. Using color doppler, flow can be visualized as the color jet passing across the septum.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Ventricular Fibrillation
A middle aged male presents to the ED in cardiac arrest. Pre-hospital assessment showed asystole and AED indicated no shock advised. Subcostal echo revealed a quivering left ventricle indicative of fine ventricular fibrillation.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Takotsubo Cardiomyopathy
A 50 year old male with community acquired pneumonia presented to the ED with worsening symptoms, abnormal EKG, and elevated troponin without an obstructing lesion on cath. Bedside echo revealed akinesia of the entire mid and apical left ventricle indicative of Takotsubo cardiomyopathy on apical 2 chamber (left) and apical 4 chamber (right) views.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Drug-induced Cardiomyopathy
52-yo-male with PMH methamphetamine use presented with 1 month history of increasing DOE, orthopnea, and episodic atypical sharp chest pain. EKG revealed LVH with inferolateral T-wave inversions; troponin was indeterminate (making ACS less likely). POCUS demonstrated extremely reduced LVEF leading to a diagnosis of new systolic heart failure. Subsequent formal TTE demonstrated LVEF 10%; left heart cath revealed nonobstructive CAD. Final diagnosis of methamphetamine induced cardiomyopathy was made.
Mike Heffler, MD
Denver Health Emergency Medicine
Atrial fibrillation
A 60-year-old female presented with palpitations; found to have atrial fibrillation. Parasternal long POCUS was notable for both an enlarged LA as well as depressed LV systolic function. These concurrent diagnoses enabled initiation of proper rate-control while also being mindful to not worsen HF exacerbation (avoiding b-blockade). The combination of A.fib as well as LV dysfunction also made this patient particularly high risk of thromboembolic events; she was therefore also initiated on therapeutic anticoagulation.
Shahad Al Chalaby, MD. PGY-2, Internal Medicine
Highland Hospital, Almeda Health System, Internal Medicine Residency Program. CA, USA
@shahad_Chalaby
Cardiac Standstill
A patient presented with out-of-hospital cardiac arrest. POCUS was used to confirm presence of cardiac standstill. Note the absence of movement of the left ventricular free wall.
Melissa Myers, MD. Emergency Medicine in Texas. Ultrasound Fellowship Program Director.
@melissamyersmd
LV Thrombus
A 50-year-old male presented to the ED with signs/symptoms of acute ischemic cerebrovascular accident (hemiplegia and dyslalia). Head CT confirmed the presence of a subacute ischemic event. Bedside POCUS (apical four chamber view) revealed severe LV global hypokinesis and the presence of an apical thrombus; the likely etiology of his cardioembolic event.
Renato Temabli, EM Physician Brazil
@JediPocus
LV Failure
Pictured is an apical 2 chamber view from a 60-year-old female who presented to our ED with acute hypoxic respiratory failure. Note the presence of LVH and LV systolic dysfunction. PLAX view additionally confirmed the presence of critical aortic stenosis; lung views were notable for >3 B-lines per frame; all consistent with her clinical picture of acute cariogenic pulmonary edema.
Guillermo A. Obregon MS-4. Central Michigan University Emergency Medicine Residency
Additional contributors: Brian Brazeau MD, Harrison Zeitler MD, Therese Mead DO, RDMS, FACEP
Takotsubo Cardiomyopathy in a Patient with Chest Pain
The Case:
A 45 year old with history of diabetes presented with chest pain and shortness of breath. Cardiac #POCUS demonstrates LV apical ballooning with basal hypercontraction consistent with Takotsubo. This was confirmed with normal coronaries on cardiac cath.
Image courtesy of IUEM Ultrasound
Original Twitter Post can be found here.
Reverse Takotsubo Cardiomyopathy
A 52-year-old female presented to the ED with acute onset of upper abdominal pain and cough productive of frothy, pink sputum. She was ill-appearing, tachypneic, tachycardic, and hypotensive. POCUS revealed severe hypokinesis of the LV basal wall with a hyperdynamic apex, and diffuse B lines in both hemithoraces. She was in cardiogenic shock secondary to basal (aka reverse) Takotsubo cardiomyopathy (TCM). This variant accounts for only ~3% of TCM cases. Interestingly, 6 months ago she suffered from the typical (apical) variant. The recurrence rate in the 1st year is ~1.5%, but having a different variant is even more rare! (The U/S clip has been slowed down to make it easier to visualize the RMWAs.)
Dr. Sam Cochran
Decreased EF (Parasternal Short)
An elderly gentleman w/ non-ischemic cardiomyopathy 2/2 meth use and a very poor EF. EPSS was 2.21 when measured in parasternal long axis correlating with severely reduce ejection fraction.
Greg Powell, MD - ULCA/Harbor
Reduced EF (Apical 4 Chamber)
An elderly gentleman with non-ischemic cardiomyopathy 2/2 meth use and a very poor EF. EPSS was 2.21 when measured in parasternal long axis correlating with severely reduce ejection fraction.
Greg Powell, MD - ULCA/Harbor
Ventricular Fibrillation
Elderly F w/ PMHx HTN and metastatic cancer arrived as a notification for sudden, witnessed syncope. EMS found PEA on EKG, intubated her, delivered 1 shock by AED, and obtained ROSC after 2 rounds of Epi. During transport she became pulseless again, and a 2nd ROSC was achieved w/ Epi in ED. During pulse check echo was used to evaluate for organized cardiac activity. Echo revealed a mild pericardial effusion w/o tamponade in PLAX, normal cardiac architecture, and absence of organized atrial and ventricular contractions. Disorganized ventricular movement correlated w/ VFib on the monitor.
Rescuer pulse palpation is only 78% accurate according to Tibballs and Russell (2008). POCUS in cardiac arrest allows for the assessment of organized cardiac activity w/o a palpable pulse, and for further evaluation of the Hs and Ts in PEA arrest. Given the need to maintain coronary perfusion w/ high quality CPR, the PLAX view is typically the fastest, provides actionable information and can be performed during standard ACLS pulse checks.
Tibballs J, Russell P. "Reliability of pulse palpation by healthcare personnel to diagnose paediatric cardiac arrest." Resuscitation 2008; 78: 135-40.
Submitted by Paul Pukurdpol, MD @PaulyPocket
Decreased EF (Parasternal Long)
An elderly gentleman w/ non-ischemic cardiomyopathy 2/2 meth use and a very poor EF. EPSS was 2.21 when measured in parasternal long axis correlating with severely reduce ejection fraction.
Greg Powell, MD
Reduced Ejection Fraction (Parasternal Long-Axis View)
Parasternal long axis with cardiomyopathy, pericardial effusion, and decreased EF.
Dr. Gordon Johnson MD
Internist
Portland Oregon & Uganda
Takotsubo's Cardiomyopathy
WCUME 2017 Submission for "Best POCUS"
Bedside Echo of patient with Takotsubo's Cardiomyopathy and a regional tamponade where the effusion is not visible in the parasternal long.
Dr. Evan Baines - Augusta, Georgia
Apical Ballooning
A 50 years old, complaining of dyspnoea and chest pain. She had no prior history of cardiopulmonary disease. Initial ultrasound of the lung fields demonstrated plenty of B-lines bilaterally.
An apical cardiac view (view is flipped with LV on left side of screen) demonstrates hypokinesis & aneurysmal dilation of the apex consistent with Takotsubo's cardiomyopathy. The patient's heart failure was managed supportively and a catheterization was performed during hospitalization that showed normal coronary artery stenosis. She had a full recovery
Ilan Ben-Shabat
5th year medical student
Aspiring emergency physician
Apical Ballooning 2
A 50 years old, complaining of dyspnoea and chest pain. She had no prior history of cardiopulmonary disease. Initial ultrasound of the lung fields demonstrated plenty of B-lines bilaterally.
An subxiphoid cardiac view demonstrates hypokinesis & aneurysmal dilation of the apex consistent with Takotsubo's cardiomyopathy. The patient's heart failure was managed supportively and a catheterization was performed during hospitalization that showed normal coronary artery stenosis. She had a full recovery
Ilan Ben-Shabat
5th year medical student
Aspiring emergency physician
Moderately Reduced Ejection Fraction - Basal Parasternal Short Axis
This image is a basal parasternal short axis view demonstrating a moderately reduced ejection fraction
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al. (Dr. Vahtrick)
Hyperdynamic Left Ventricle (Short)
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al. (Dr. Fares)
Severe Left Ventricular Failure
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al. (Dr. Kaveh Kaynama)
Severely Reduced EF
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al.
Ventricular Fibrillation
Disorganized cardiac activity consistent with ventricular fibrillation.
Sukh Singh, MD
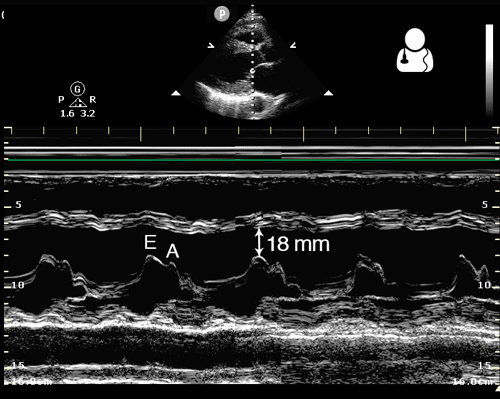
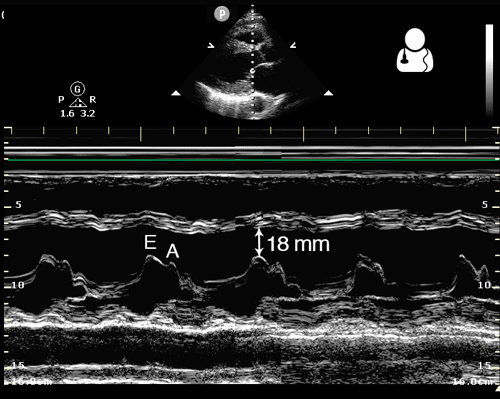
Abnormal End Point Septal Separation (EPSS)
One way to evaluate cardiac function is to measure the distance from the anterior leaflet of the mitral valve to the septum during diastole. This is known as end point septal separation (EPSS).
An EPSS < 7 mm is considered normal, while EPSS > 10 mm suggests decreased cardiac function.
This measurement should be obtained in a parasternal long axis view, using M-mode with the cursor placed through the tip of the mitral valve.
Image credit: Ultrasound of the Week
Reduced LV Function
60s M with no known PMH presented to the ED with 3 weeks of progressive dyspnea and bilateral leg edema. POCUS was performed to assess his cardiac function. This clip demonstrates the parasternal long axis and apical 4-chamber views, showing markedly globally reduced LV function, and the endocardium is well seen here. The patient was admitted for further evaluation of his newly diagnosed cardiomyopathy, and formal echocardiography revealed a subtle apical LV thrombus which is not well seen on this POCUS.
Dr. Matthew Riscinti
Denver Health Medical Center
Septal Dyskinesis (Subcostal View)
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al.
Bi-ventricular Failure in Vasculitis
24-yo-male who had been diagnosed with granulomatosis with polyangiitis 10 months prior presented with DOE and progressive bilateral lower extremity edema. Clinical suspicion of cardiac dysfunction was confirmed by POCUS; seen here is the apical 5-chamber view, nearly unable to fit on screen due to severity of bi-ventricular dilation and impaired systolic function.
Tessa W. Damm, DO
Intensivist, Critical Care Medicine & Neurocritical Care.
Wisconsin, USA
@DrDamm
Biventricular Failure Parasternal Long
50 y/o M PMH methamphetamine abuse presents in respiratory failure with cool, mottled skin and poor capillary refill. Patient was tachycardic, hypothermic with multiple signs of end organ dysfunction. POCUS quickly narrowed the differential by demonstrating clear, severe, reduced ejection fraction by visual estimation and a plethoric IVC without respiratory variation. Patient was ultimately started on dobutamine and transferred to the MICU for treatment of cardiogenic shock.
Dr. Jaclyn Walker, Dr. Matthew Riscinti - Denver Health Emergency Medicine
Biventricular Failure Apical 4
50 y/o M PMH methamphetamine abuse presents in respiratory failure with cool, mottled skin and poor capillary refill. Patient was tachycardic, hypothermic with multiple signs of end organ dysfunction. POCUS quickly narrowed the differential by demonstrating clear, severe, reduced ejection fraction by visual estimation and a plethoric IVC without respiratory variation. Patient was ultimately started on dobutamine and transferred to the MICU for treatment of cardiogenic shock.
Dr. Jaclyn Walker, Dr. Matthew Riscinti - Denver Health Emergency Medicine
Parasternal Short Axis: Sepsis-induced cardiomyopathy
Seen here is a parasternal short-axis view from a patient who presented with sepsis. POCUS was notable for sepsis-induced cardiomyopathy.
Johannes Achenbach
Sepsis-Induced Cardiomyopathy
Pictured is an apical 4 chamber view of a patient who presented with sepsis secondary to lobar pneumonia and was found to have sepsis-induced cardiomyopathy. Appreciate both LV and RV systolic dysfunction.
Johannes Achenbach
Hyperdynamic State
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al. (Dr. Fares)
Hyperdynamic State (Long)
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al. (Dr. Fares)
Asystole
Fluid bubbles sitting in right ventricle without any signs of cardiac activity. Imaging taken during cardiac arrest resuscitation pulse check.
Sukh Singh, MD
Cardiac Arrest with Agonal Rhythm
Justin Bowra MBBS, FACEM, CCPU Emergency Physician, RNSH et al.
Asystole
Out of hospital arrest brought in by EMS. CPR had been ongoing for 20 minutes without ROSC. Parasternal short axis view at mid papillary level shows complete LV standstill once resuscitation was stopped, confirming the clinical diagnosis.
Dr. Cian McDermott - Mater University Hospital Dublin, Ireland
Regional Wall Motion Abnormality
60s M presented with L arm and axillary pain for 1 day. EKG with subtle ST elevation in II/III and depression in I, aVL without meeting STEMI criteria. HsTrop elevated to about 25,000. POCUS demonstrated hypokinesis of the inferior and lateral walls. Cardiology felt most c/w NSTEMI and missed inferior MI. TTE confirmed regional wall motion abnormalities, and after medical optimization, pt went to cath lab and had RCA occlusion diagnosed and stented.
Dr. Spencer Seballos, PGY1
Denver Health Residency in Emergency Medicine