Orbital
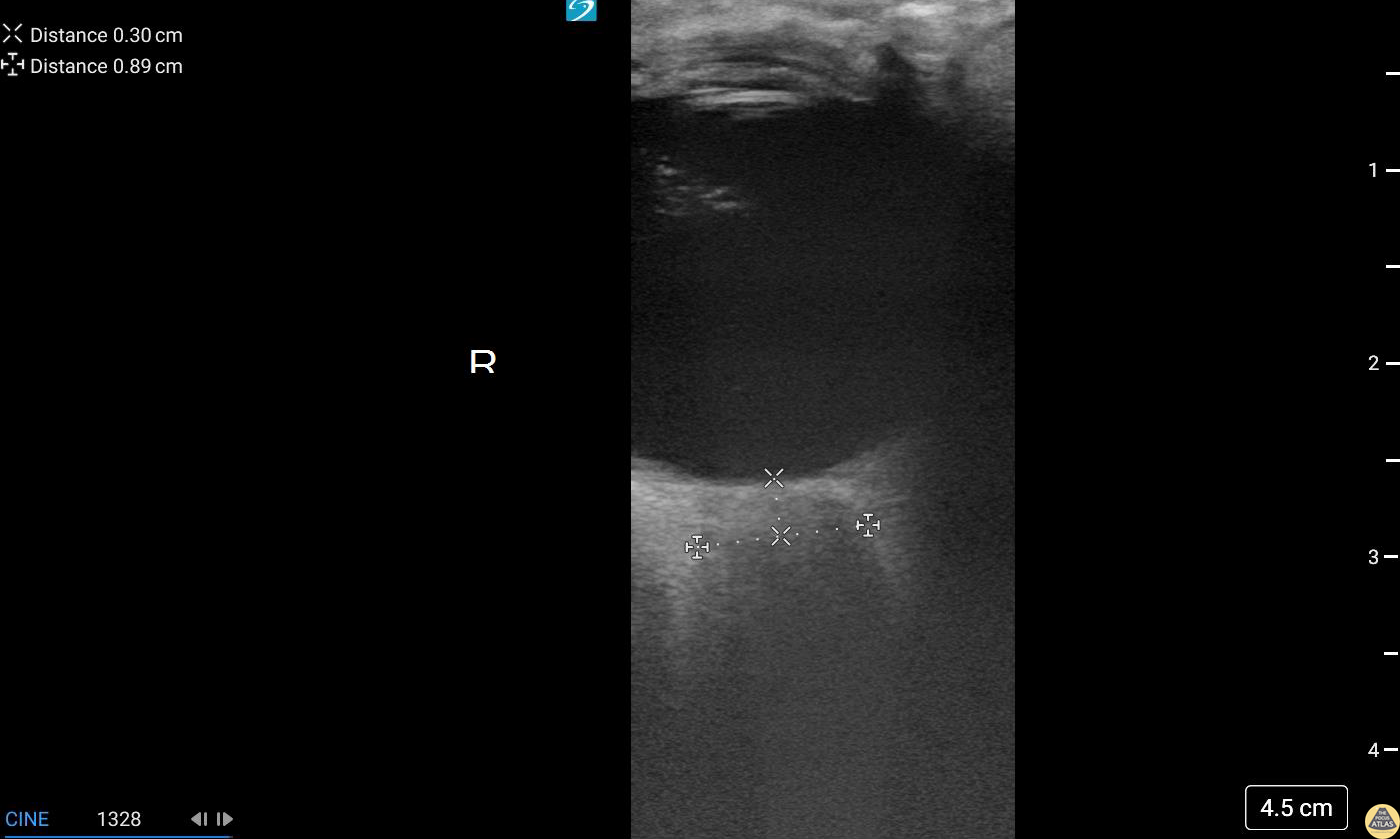
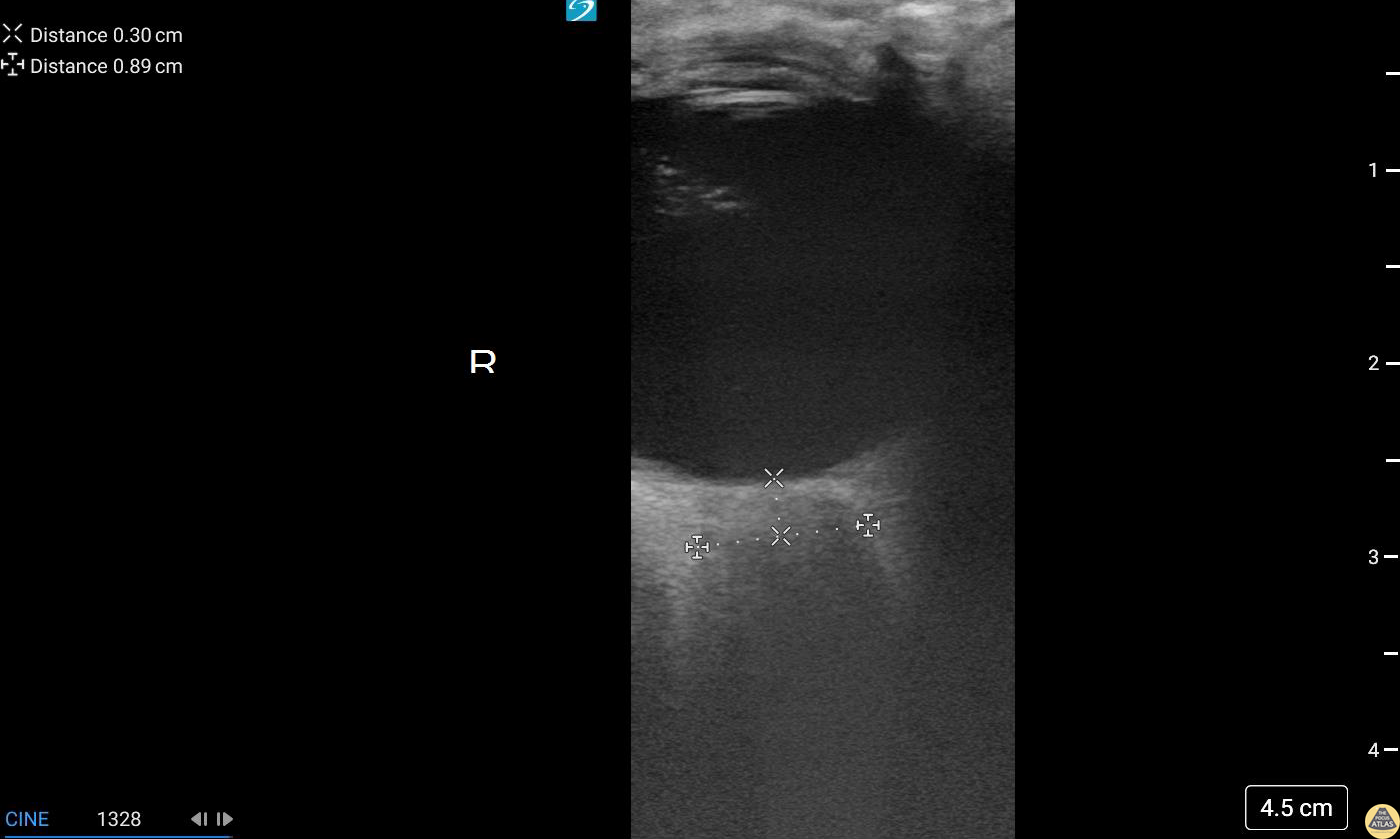
Retinal Edema (2/2 - Clip)
17 y/o female with sudden onset bilateral blurry vision after prolonged indoor cat exposure. Fundoscopy showed retinal pigment epithelium loss consistent with bilateral neuroretinitis from cat scratch disease (Bartonella henselae).
The hyperechoic retina, normally flush with the posterior aspect of the globe, is seen separated by a hypoechoic band of edema.
Retinal edema from cat scratch disease is rare (Gen Opth 19th ed. 2017:378-422), but can be diagnosed by POCUS.
Contributed by: John Hipskind, MD, Ultrasound Director, Kaweah Health EM Residency
Retinal Edema (1/2 - Still)
17 y/o female with sudden onset bilateral blurry vision after prolonged indoor cat exposure. Fundoscopy showed retinal pigment epithelium loss consistent with bilateral neuroretinitis from cat scratch disease (Bartonella henselae).
The hyperechoic retina, normally flush with the posterior aspect of the globe, is seen separated by a hypoechoic band of edema.
Retinal edema from cat scratch disease is rare (Gen Opth 19th ed. 2017:378-422), but can be diagnosed by POCUS.
Contributed by: John Hipskind, MD, Ultrasound Director, Kaweah Health EM Residency
Intraoccular Lens Subluxation
A 50 year old male with a prior history of bilateral intraoccular lens (IOL) transplants presented to our ED with sudden onset foggy vision in his right eye while getting out of the shower. He was unable to participate in visual acuity due to the extent of his blurred. POCUS demonstrated “iridodonesis” and a provisional diagnosis of IOL subluxation/dislocation was made. Ophthalmology was consulted and confirmed the diagnosis.
Dr. Piaseczny, PGY4 Emergency Medicine, Queen's University, Kingston, Ontario, Canada
Prosthetic Ocular Lens Subluxation
This patient presented with decreased vision on a background of advanced macular degeneration. VA in the eye had decreased from 20/150 to 20/400 on presentation.
Interestingly the patient stated "I think my ocular lens has displaced."
Contributed by: Colin Bell, FRCPC, DPSPC
Phthisis Bulbi secondary to end stage eye disease
93 year old male with established end stage eye disease found incidentally to have prominent Phthisis Bulbi made evident by a heterogeneous hyper-echoic structures (calcifications) within the posterior chamber of the left eye.
Contributed by: Davis, Lindsay; Schlangen, Alex; Welch, Matthew

Papilledema From Optic Pathway Glioma
A 24-year old male presented to the ED with a six-month history of progressive total right vision loss. A bedside ocular ultrasound examination was performed that revealed an elevated optic disc with enlarged ONSD measuring 9.7mm, consistent with papilledema. An MRI of the head confirmed an enlarged intraconal portion of the right optic nerve, consistent with glioma.
Marko Lubardic, MS4; Tom Taugher, DO, PGY3; Michael Bernard, DO, PGY1; Central Michigan University Emergency Medicine Residency
Old Globe Rupture
Irregularly shaped eye with internal dense structure concerning for intraocular hematoma. This patient had a history of previous rupture of the globe.
A CT Head without IV contrast described the left eye as follows: Small left globe with high density concerning for intraocular hemorrhage. Direct examination is recommended.
Halimah Hamidu-Egiebor Central Michigan University College of Medicine MD-MBA '24, Arthur Sieron Central Michigan University Emergency Medicine Resident, Eric 'Dax' Spencer Central Michigan University Emergency Medicine Resident
Vitreous Detachment
This was from a 52 year old male with a recent surgical history of vitreous detachment that became a retinal detachment. He presented to the emergency room for vision changes in same eye after an object fell and hit his head. Ocular ultrasound was performed at the bedside which revealed a new vitreous detachment. Important to note here that it is crucial to fan/tilt through the entire eye, making sure to visualize the optic nerve in order to differentiate between a vitreous and retinal detachment. In this case, notice how the lesion spotted in the chamber does not connect to the optic nerve, which is consistent with a vitreous detachment.
Dr. Christopher Paulo, DO, PGY-1
Riverside Regional Medical Center Emergency Medicine Program (Newport News, VA)
Central Retinal Artery Occlusion
This is from a 63 year old female who initially presented to the emergency department with vision loss over the last 24 hours. She reported bending over when she experienced complete vision loss from one of her eyes. Point of care ultrasound was performed, locating the optic nerve, but more interestingly a hyperechoic structure within the nerve (spot sign).
Overall, this is was suggestive of a central retinal artery occlusion. In this sort of situation, color doppler can also be utilized to assess for arterial versus venous occlusion.
Dr. Christopher Paulo, DO, PGY-1
Riverside Regional Medical Center Emergency Medicine Program (Newport News, VA)
Orbital Endophthalmitis
A 43 year old male with 3 days of painful right eye vision loss, fever, and URI symptoms presented to the emergency department. POCUS demonstrates echogenic swirl within the vitreous cavity. The patient was diagnosed with endogenous endophthalmitis caused by Klebsiella Pneumoniae.
Contributor: Hyun J. Yi (John), D.Sc, PA-C, MAJ, USA, Emergency Ultrasound Fellow, Madigan Army Medical Center, Joint Base Lewis-McChord, WA
Enlarged Optic Nerve
A 75 year old male with history of ocular melanoma and blindness of the right eye presented for right sided headache and nausea for the past 2 days.
Ocular US was performed demonstrating significant enlargement of the optic nerve sheath.
Contributors: Michael Bernard, DO; Thomas Taugher, DO; Marko Lubardic
Central Michigan University Residency of Emergency Medicine
Lens Subluxation
Middle aged male with prior bilateral lens replacement presented with atraumatic vision loss. POCUS performed that demonstrates subluxed lens without retinal detachment. Discussed with ophthalmology and pt was discharged with 24 hour follow up with ophthalmology, with eventual plan for operative repair.
Michael Maurantonio, PGY3, Denver Health Residency in Emergency Medicine
Michael Del Valle, Fellow, Denver Health Ultrasound Fellowship
Metallic Foreign Body In Orbital Soft Tissue
This is a clip from a patient presenting with foreign body sensation. They had a piece of metal hit their eye a week ago. Previously seen for complaint but told no foreign body seen on exam.
On ultrasound clip a hyperechoic structure can be seen adjacent to the globe. Note that with dynamic eye movements the foreign body does not move suggesting this is outside of the globe.
Image courtesy of Robert Jones DO, FACEP @RJonesSonoEM
Director, Emergency Ultrasound; MetroHealth Medical Center; Professor, Case Western Reserve Medical School, Cleveland, OH
View his original post here
Anterior Lens Dislocation and Retinal Detatchment
46 yo woman pmh multiple right eye surgeries presenting with atraumatic left eye pain, decreased vision, and mydriasis, which was initially concerning for acute angle-closure glaucoma. POCUS revealed anterior lens subluxation given the very shallow anterior chamber. Around 5% of acute angle-closure glaucoma is induced by lens subluxation. Retinal detachment, the hyperechoic line in the far field, can also be seen on POCUS. Ophthalmology successfully treated her with lensectomy and secondary intraocular lens implantation.
Robert Adrian
Ruptured Globe
This patient sustained blunt trauma to the eye from a fireworks injury. CT scan performed prior to POCUS showed intra-orbital hematoma and complete absence of any globe tissue. The patient was taken to the OR for primary enucleation, washout, and closure.
Earl “Quinn” Cummings, MD @resus_bae
Assistant Professor; MUSC Emergency Medicine/Ultrasound; MUSC Pediatric Emergency Medicine
Retinal Detachment
Retinal Detachment.
Francisco Norman
Vitreous Hemorrhage
An 81 yo female on ASA presented with 6 hour hx of blurred vision in her right eye. Ocular POCUS demonstrated a hyperechoic clot, seen here as 'swirling' movement, with debris settling near the bottom of the globe when eye is not in motion (end of clip). In early presentation of vitreous hemorrhage when blood is still liquified, increasing the ultrasound gain can greatly assist with identification of pathology.
Mandy Peach, MD @mandy_peach
Saint John Regional Hospital. NB, Canada
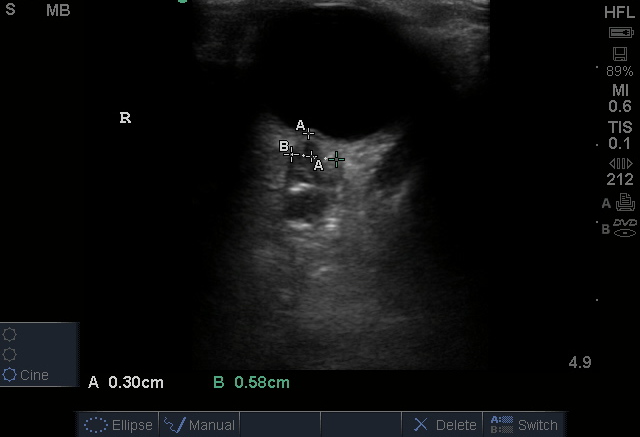
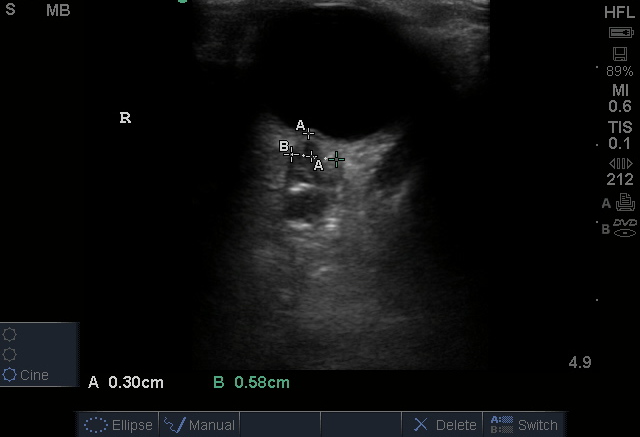
Normal ONSD
A 35 yo female presented to a rural ED with worsening headache accompanied by nausea/vomiting after failed treatment for sinusitis. The department did not have immediate access to CT scanning, therefore Optic Nerve Sheath Diameter (ONSD) was used to assess for associated increased intracranial pressure. The optic nerve sheath is contiguous with the subarachnoid space, making ONSD an indirect measure of intracranial pressure. Visualize the hypoechoic optic nerve posterior to the globe and measure 3mm back from the globe (calipers A) to determine site of measurement . Then measure to the edges of the sheath (calipers B) horizontally. Value >5mm is concerning for increased ICP. This ONSD is normal.
Mandy Peach, MD @mandy_peach
Saint John Regional Hospital. NB, Canada
Vitreous Hemorrhage due to Proliferative Diabetic Retinopathy
A 70-year-old man presented with loss of vision to his right eye (hand motion and light perception). He takes warfarin and has diabetes. Monocular vision loss triggered a POCUS that revealed a hazy echogenic substance (consistent with blood) seen best when patient activates extra-ocular muscle movements. Also note the associated bright linear structure within one portion of the bleed, the hyaloid membrane. This patient was subsequently assessed by the Eye Hospital and diagnosed with vitreous hemorrhage due to proliferative diabetic retinopathy.
Peter Cheng
Retrobulbar Hematoma
Patient experienced ocular trauma 3 days prior to this exam, having been struck with a baseball to the eye. Notice the hypoechoic area within the retrobulbar space, consistent with a retrobulbar hematoma.
Tomasz Przednowek & Jereme Long @jplongest
Vitreous Hemorrhage
A 71-year-old male with a history of hypertension and diabetes presented to the ED reporting gradual vision loss in his right eye over a 3-day period. Physical exam was notable for a 3 mm and nonreactive pupil with ipsilateral visual acuity reduced to patient only being able to detect movement. POCUS revealed swirling echodensity within the right eye, most appreciable with extraocular muscle movements. Ophthalmology subsequently confirmed our suspected diagnosis of vitreous hemorrhage.
Richard Cunningham, MD @HappyDays_EM
Maricopa Medical Center
Endogenous Endophthalmitis
A middle aged female with ESRD and longstanding percutaneous HD catheter with recent MSSA bacteremia was admitted with septic shock. She subsequently developed subacute bilateral visual loss (OS > OD). Clinical suspicion of endogenous endophthalmitis was initially supported by POCUS notable for heterogenous intraoccular material within vitreous. She was immediately started in intravitreal antibiotics in addition to previously initiated systemic antibiotics. Diagnosis of endogenous endophthalmitis was subsequently confirmed by vitrectomy.
Tessa W. Damm, DO
Intensivist, Critical Care Medicine & Neurocritical Care.
Wisconsin, USA.
@DrDamm
Spontaneous Retinal Detachment
30s M with no known medical history or ocular history presented with 2 days of progressive monocular visual field deficits and floaters without antecedent trauma or other injury. Visual acuity was limited to finger counting at 3 feet in the affected eye. POCUS of the affected eye is shown here, demonstrating a macula-off retinal detachment. The patient was seen by ophthalmology and had urgent surgery the next morning.
Dr. Amy Allen, PGY1
Denver Health Residency in Emergency Medicine
Asteroid hyalosis (an ultrasonographic mimic of vitreous hemorrhage)
An 59-year-old male with PMH of ESRD presented with 10-day hx floaters in his right eye. Sonographic findings are shown, notable for multiple, mobile, hyperechoic densities that swirled rapidly with eye movement. The appearance is similar to that of vitreous hemorrhage.
The patient was subsequently evaluated by ophthalmology who confirmed a diagnosis of asteroid hyalosis; a rare, benign condition of calcium phospholipid deposition within the vitreous fluid. The sonographic findings are so similar to vitreous hemorrhage that the two are commonly mistaken for each other. The clinical differentiation is that asteroid hyalosis is most often asymptomatic, and almost always without visual deficits (possibly benign floaters). These patients also rarely require vitrectomy.
In addition to clinical presentation, asteroid hyalosis can be differentiated from vitreous hemorrhage by subtle sonographic features. In asteroid hyalosis, the hyperechoic calcium phospholipid particles have a sparkling, "starry sky" appearance compared to the typically duller heterogenous blood seen in vitreous hemorrhage.
Vicky Lam, MD, MS; Christianna Sim, MD; Olusola Sanusi, MD
Kings County Hospital, SUNY Downstate Emergency Medicine
Retrobulbar Hematoma
A 65-year-old patient presented with sudden-onset headache with associated right eye pain and diplopia. Physical exam also notable for an unsteady gait, exophthalmus, and impaired EOM including absent upward and medial gaze of right eye. Orbital POCUS revealed a retrobulbar hematoma causing external compression of the optic nerve.
Marco Garrone, Emergency Medicine Physician
@drmarcogarrone
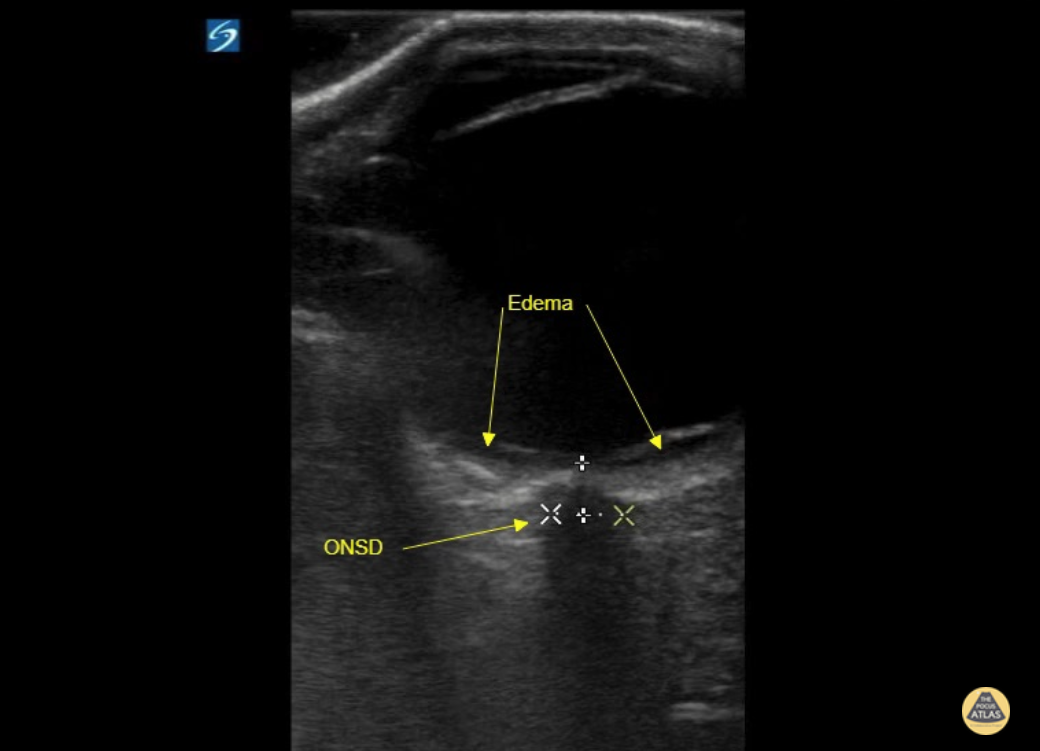
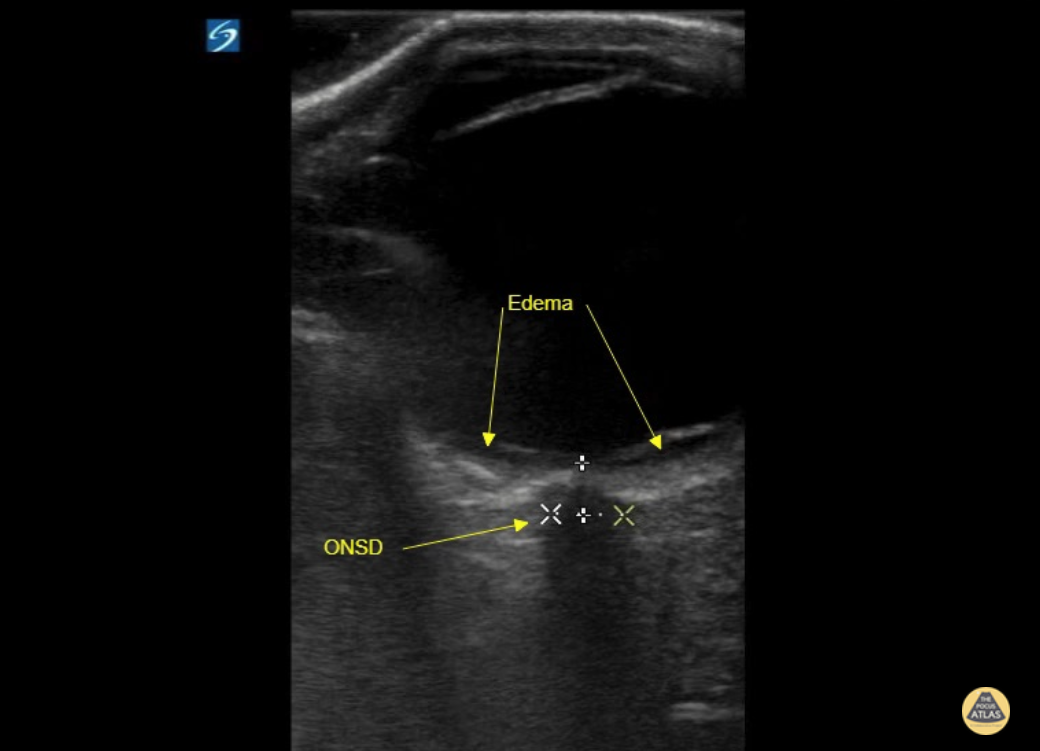
ONSD Double Take
We used OSND to evaluate a patient with COVID-19 encephalitis and found evidence of increased intracranial pressure (ICP). Note, due to the high frequency probe used, we were able to appreciate fine detail including two hypoechoic boarders at each lateral edge of the optic nerve. It is the most lateral outer edge/ hypoechoic structure that represents the optic nerve sheath.
Eric M. Siegal, MD, SFHM, FCCM
Aurora Critical Care Service; Milwaukee, WI
Adjunct Clinical Professor of Medicine University of Wisconsin School of Medicine and Public Health
ONSD normal ICP
Patient presented with fall from standing height with resultant traumatic subarachnoid hemorrhage (SAH). POCUS of ONSD is reassuring in that ONSD is <5 mm, suggestive of no associated elevated intracranial pressure.
Tessa W. Damm, DO. Intensivist. Milwaukee, WI
@DrDamm
ONSD for ICP
A patient presented with spontaneous intracranial hemorrhage (ICH) secondary to arteriovenous malformation (AVM). She reported severe HA for 3 days with progressive somnolence and associated vomiting. Assessment of her ONSD revealed a width just >5 mm, consistent with an elevated intracranial pressure (ICP).
Tessa W. Damm, DO. Intensivist. Milwaukee, WI
@DrDamm
Papilledema
A 27 year-old female presented to the emergency department with a two week history of headache, posterior eye pain, and visual changes. A bedside ultrasound was performed demonstrating a dilated optic nerve sheath and a bulging optic disc protruding into the posterior chamber consistent with papilledema. A CT of the head was unremarkable and an LP was performed with opening pressure of 36 mmH2O consistent with intracranial hypertension.
Image courtesy of Dr. Amir Aminlari
Ultrasound Fellowship Director, University of California San Diego
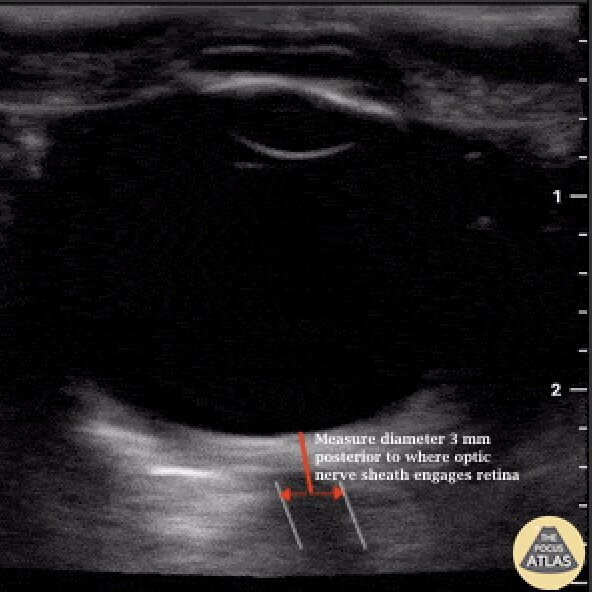
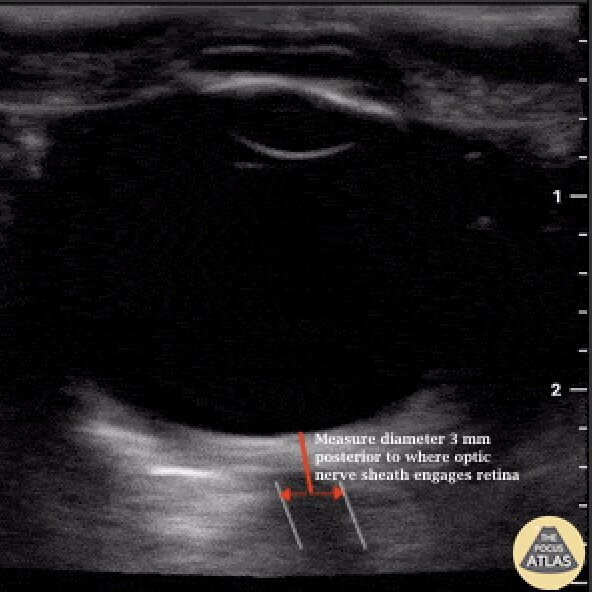
Measuring Optic Nerve Sheath Diameter
When evaluating for elevated intracranial pressure using optic nerve sheath diameter, (ONSD), proper measurement should be obtained 3 mm posterior to where the optic nerve engages the retina.
Image courtesy of Dr. Tessa Damm (@DrDamm)
Lense Replacement
60 year-old woman with longstanding history of severe cataracts presenting 5-months s/p cataract extraction with intraocular lens placement (CEIOL). Ultrasound exam demonstrates a linear echogenic structure posterior to the iris with reverberation artifact in place of normal lenticular structure (native lens) consistent with artificial lens.
Image acquired by Robert J. McMickle (Medical Student IV, UCLA) under guidance of Yiju Teresa Liu, M.D., RDMS at Harbor-UCLA Medical Center.
Consensual Light Reflex
Seen is the constriction of the Pupillary Sphincter when a light is shone on the contralateral pupil, demonstrating the Consensual Pupillary Reflex. In the setting of severe Orbital trauma and swelling, POCUS may be used to assess this reflex arc. Dysfunction in the arc may be associated with pathology at the Retina, Midbrain, Optic, and/or Oculomotor nerve.
Dr. Mohamed Elfatihi and Dr. Surriya Ahmad - Kings County Emergency Medicine
Posterior Vitreous Hemorrhage
Posterior Vitreous Hemorrhage
Painless visual field cut with position change. Posterior vitreous hemorrhage with organization and dynamic movement gong over the top of the optic nerve, but not involving it to suggest retinal detachment.
Dr. Dustin Morrow
Orbital Abscess
Orbital cellulitis evolving into abscess in diabetic patient. Multiple pus collections are visible on the medial side.
Dr. Marco Garrone
Looking Around - Normal Exam
Normal ocular ultrasound over closed eyelid as patient moves eye medially and laterally.
Sukh Singh, MD
Retinal Detachment
Here a hyperechoic linear density is seen arising from the location of the fundus, indicating retinal detachment. Posterior vitreous detachment and vitreous hemorrhage can look similar to retinal detachment. Given the imminent risk of blindness in these conditions it is essential to identify them as soon as possible. POCUS is an excellent way to do so given the time and skills required to perform a proper fundoscopic exam. Literature has shown sensitivity for this test to be 97-100% and specificity 83-100%. So next time ask yourself... is your fundoscopic exam that good?
Sukh Singh, MD
Retinal Detachment with Vitreous Hemorrhage
34 y/o M with acute, atraumatic, painless, complete vision loss in the right eye x3 days, with an eye exam showing opacification of the right pupil and no light/dark perception. Ocular POCUS revealed a complete retinal detachment (RD) with a classic funnel shape. The funnel shape is caused by strong attachments of the retina to the optic nerve posteriorly, and to the ora serrata anteriorly.
POCUS has been shown to have sensitivity 91-100% and specificity 68-96% for RD.
In this image, the hyperechoic area within the funnel suggests an associated vitreous hemorrhage (VH), 30% of which are caused by retinal tears (RT). In fact, in patients with fundus-obscuring VH like our patient, 67% and 39% will have an associated RT or RD, respectively.
Dr. Theodore J. Segarra, Dr. Stephanie Garcia, Dr. Nayla Delgado-Torres. SUNY Downstate/Kings County Emergency Medicine.
Vitreous vs. Retinal Detachment
A 44 year old man came to ED with a shimmering effect in his left eye and unilateral temporary painless visual disturbance. He had previously been treated for a retinal tear.
Ocular PoCUS shows a frond-like linear structure lifting away from the posterior surface of the globe.
Posterior vitreous detachment (PVD) was suspected while retinal detachment (RD) was also considered. PVD was confirmed by the specialist team and the patient was treated conservatively.
Dr. Cian McDermott, Emergency Physician - University Hospital Geelong, Australia
Retinal Detachment
65 y/o F PMH DM with sudden onset flashes of light and floaters followed by progressively worse blurred vision in her right eye. She has history of cataracts surgery as well as DM retinopathy. POCUS of affected eye shows a prominent hyper-echoic linear density floating freely above the posterior fundus as shown.
Retinal Detachment is considered one of few emergencies whereby the retina becomes detached from the choroid. Once separated from the choroid’s blood supply, retinal ischemia ensues which can result in complete blindness in the affected eye. Salvage of such a potentially devastating injury relies on quick and efficient diagnosis with subsequent referral to definitive care.
Bedside ultrasound has been shown to be 100% sensitive as a screening tool for RD [AEM 2010 Sep;17(9):913-7]. Have patient close eye and place liberal amount of gel either directly over eye or atop a tegaderm dressing. Use a linear probe and scan eye in axial plane to reveal findings demonstrated above.
Dr. Eric Roseman - Kings County Emergency Medicine
Retinal Detachment
Retinal detachment in a patient with 1 day of a right sided visual field cut.Literature has shown sensitivity for this test to be 97-100% and specificity 83-100%. So next time ask yourself... is your fundoscopic exam that good?
Dr. William Scheels
Lens Dislocation
Patient with severe maxillofacial trauma of unclear etiology. Ocular POCUS demonstrates a biconvex structure with a hyperechoic rim consistent with traumatic lens dislocation.
Dr. Joshua Schechter - SUNY Downstate/Kings County Emergency Medicine
Vitreous Hemorrhage - Washing Machine Sign
47 y/o M with coronary artery disease on aspirin/clopidogrel with 4 days of decreased vision in his right eye. POCUS demonstrates swirling, amorphous echogenicities known as "the washing machine sign." If the eye remains still the blood will settle with gravity.
Fundoscopic evaluation by ophthalmology confirmed the diagnosis of vitreous hemorrhage.
Dr. Matthew Riscinti and Dr. Taylor Conrad - Kings County/SUNY Downstate Emergency Medicine
Central Retinal Artery and Venous Flow - Normal
Venous and arterial flow can be seen in this color flow doppler image.
Dr. Joshua Schechter - SUNY Downstate/Kings County Emergency Medicine
Central Retinal Artery Occlusion
Only venous flow can be appreciated in this color flow image. The central retinal artery has been occluded.
Dr. Joshua Schechter - SUNY Downstate/Kings County Emergency Medicine
Assessment Using Ultrasound for Elevated Intracranial Pressure
Elevated intracranial pressure can be assessed reliably with POCUS.
Find the optic nerve and measure 3mm back from the posterior globe. From here measure the optic nerve from inner wall to inner wall. the normal width is < 5 mm.
A systematic review and meta-analysis found POCUS has a sensitivity of 96% and specificity of 93% for increased intracranial pressure. J Ultrasound Med. 2015 Jul;34(7):1285-94. doi: 10.7863/ultra.34.7.1285.
Dr. Matthew Riscinti - Kings County/SUNY Downstate Emergency Medicine - Image from the Department of Emergency Ultrasound
Normal Eye Anatomy
This image of the eye shows the following structures, from superficial to deep: eyelid, cornea (hyperechoic), anterior chamber (anechoic), iris (hyperechoic), lens (hyperechoic), vitreous (very large anechoic area), retina (flush with the posterior wall of the globe, not visible as a distinct structure under normal conditions), optic nerve sheath (hypoechoic structure extending midline perpendicularly from the globe at the bottom of the image).
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Vitreous Detachment
40 year old male with 6 months of decreased vision from his left eye. No pmh or history of trauma. VA was obviously decreased relative to the contralateral eye. POCUS rapidly revealed a freely floating hyperechoic membrane consistent with vitreal detachment. To differentiate between a vitreous and retinal detachment you must look to see if the membrane is attached to the hypoechoic optic nerve. The retinal is continuous with the optic nerve therefore stays attached to the optic nerve in a retinal detachment. A vitreous detachment would be completely untethered as seen in this image. You can also see the “washing machine sign” better pictured in other images in this gallery.
Matt Riscinti, MD Bryan Flores, MD - Kings County Emergency Medicine
Subcutaneous Emphysema - Eyelid
Eyelid subcutaneous emphysema detected on US ocular scan
Dr. Marco Garrone

Retinal Detachment
52M PMH L cataract surgery presented with painless left eye vision loss preceded by flash. POCUS performed in the ED demonstrated a left sided retinal detachment with macula attached (“mac-on”), with retinal hemorrhage as well. Ophthalmology was consulted, and the patient was taken urgently to the OR for vitrectomy and retinal repair.
Dr. Michael Kidon, PGY3
Denver Health Residency in Emergency Medicine
Macula Off Retinal Detachment
70s F with PMH DM, HTN presented to the ED with 1 month of atraumatic, painless vision loss. Her visual acuity was limited to light perception only. POCUS was performed and is shown here. This clip of the eye is obtained with the left of the screen being medial/nasal, and the right of the screen being lateral/temporal. An irregular hyperechoic line is shown in the posterior chamber, which is attached to the optic disk, representing a detached retina. The patient’s presentation with profound painless vision loss, and detached lateral aspect of the retina is consistent with a macula off retinal detachment. Given the timeframe and POCUS findings, the patient was scheduled for urgent but nonemergent ophthalmology follow up for operative repair of the detached retina.
Dr. Cody Brevik, PGY4
Denver Health Residency in Emergency Medicine
Macula Off Retinal Detachment with Vitreous Hemorrhage
50s M with PMH cataract surgery presented with sudden onset flashing and floaters in his eye, followed by painless vision loss. His visual acuity was limited to light perception only. A still POCUS image is shown here, with an irregular hyperechoic line in the posterior chamber which is attached to the optic disc, representing a retinal detachment. Scattered hyperechoic areas are seen in the posterior chamber anterior to the retina, likely representing vitreous hemorrhage. The presentation with profound painless vision loss and retinal detachment on the medial and lateral aspects of the retina suggests involvement of the macula (“macula off” retinal detachment). This patient was evaluated by ophthalmology in the ED and was taken for operative repair.
Dr. Michael Kidon, PGY4
Denver Health Residency in Emergency Medicine