The Evidence Atlas
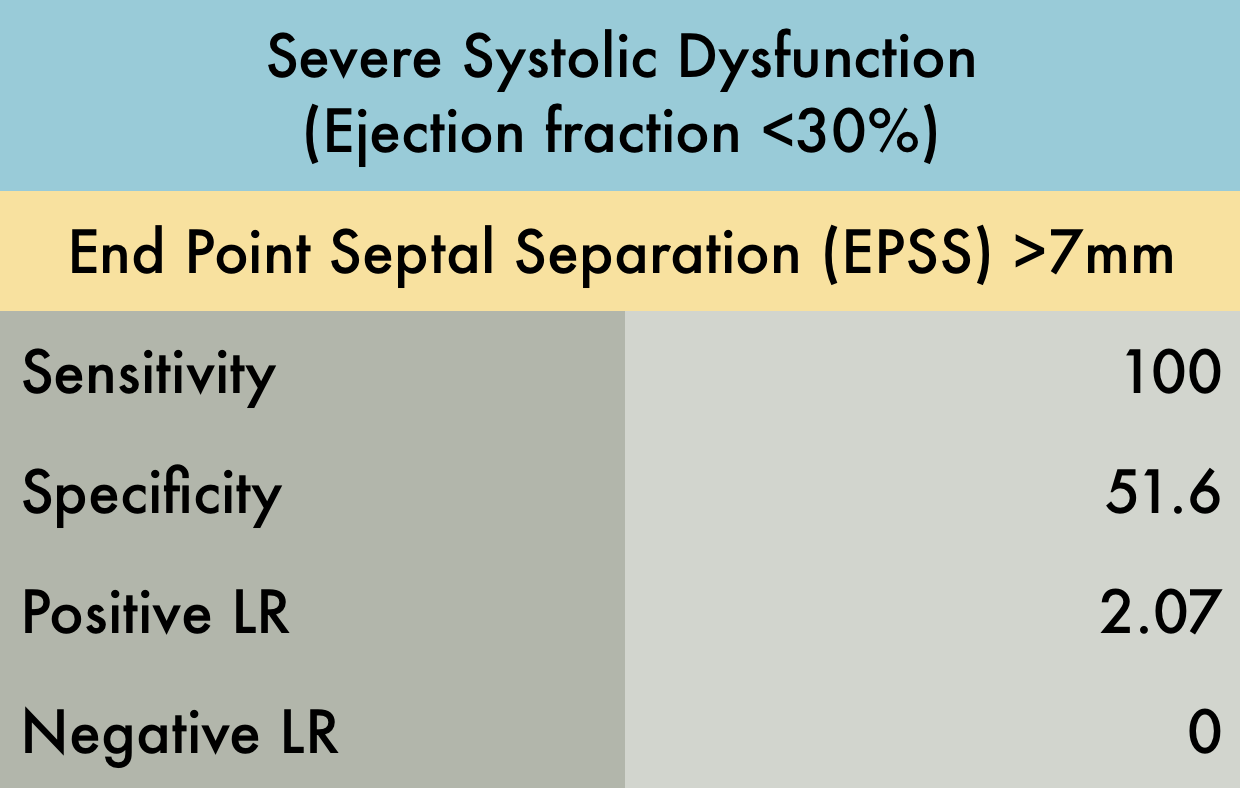
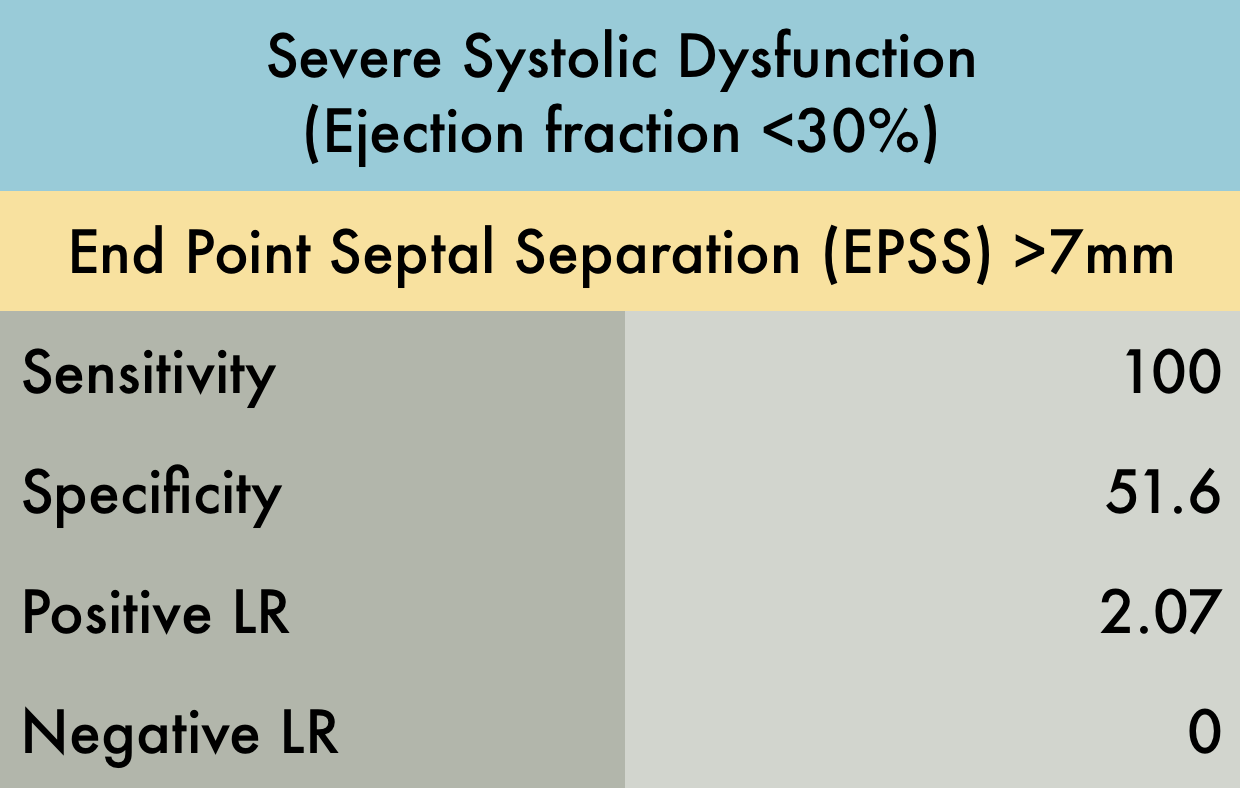
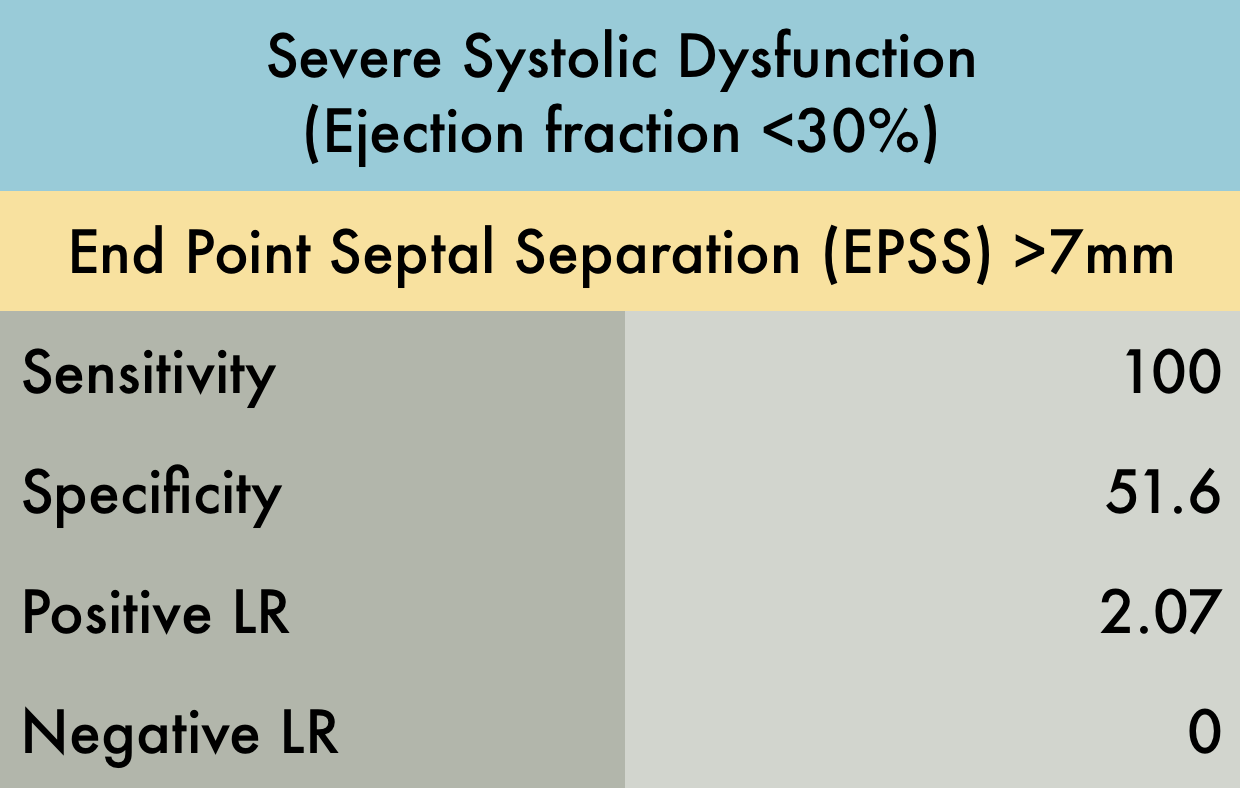
End Point Septal Separation
This was a prospective observational study (n=80) comparing emergency medicine (EM) physician performed mitral valve EPSS to formal TTE LVEF estimation. A convenience sample of unselected hospitalized patients undergoing comprehensive TTE for any indication was used. While EPSS > 7 mm was noted to be 100% sensitive for predicting severe systolic dysfunction (EF < 30%), a second cutoff of 8 mm was used for assessing any systolic dysfunction. The sensitivity and specificity of an EPSS > 8 mm for any systolic dysfunction were 83.3% (95% CI, 62.6-95.2) and 50.0% (95% CI, 29.2-70.9), respectively. The corresponding positive LR was 1.67, and the negative LR was 0.33.
PMID: 24630604
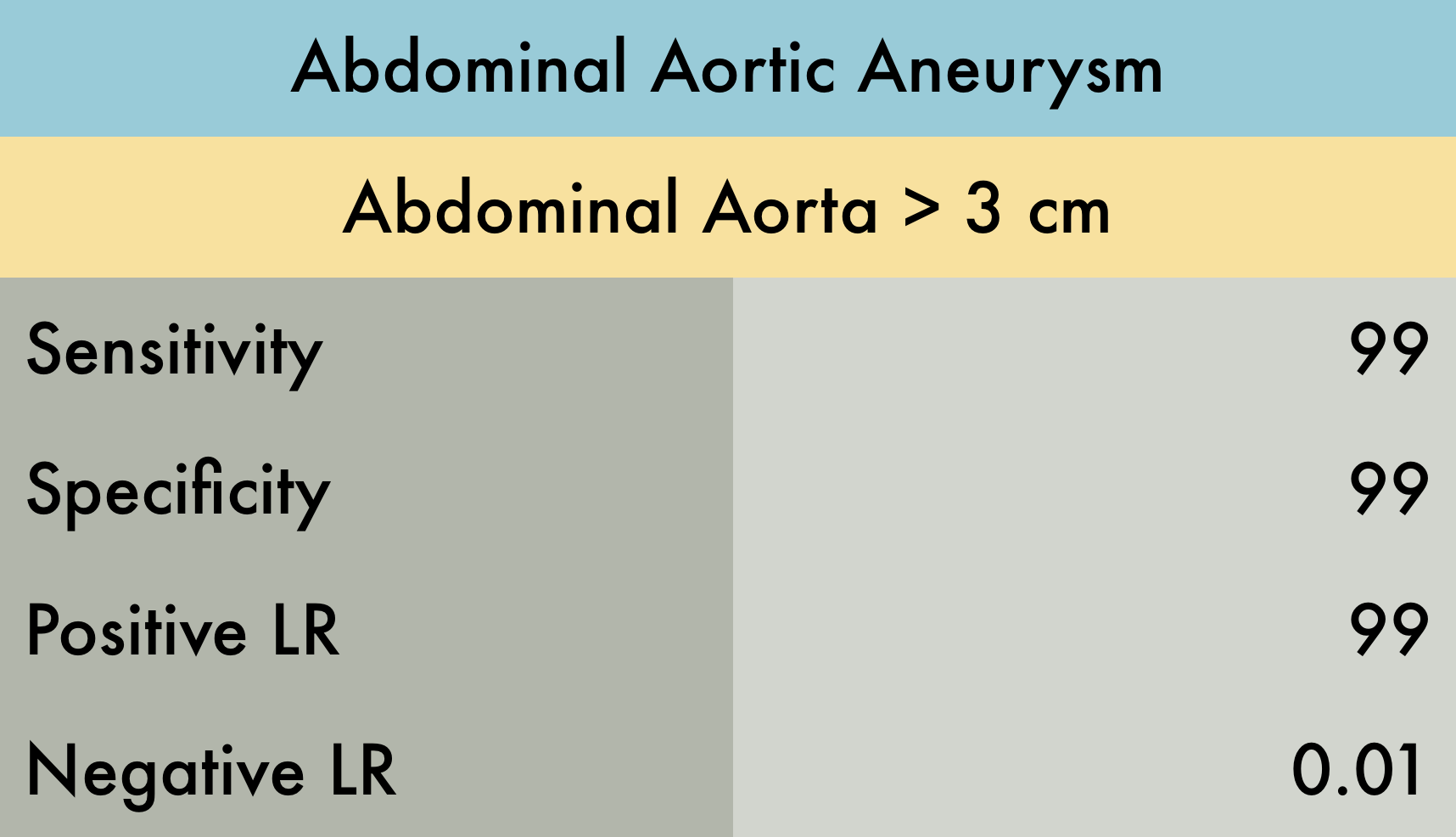
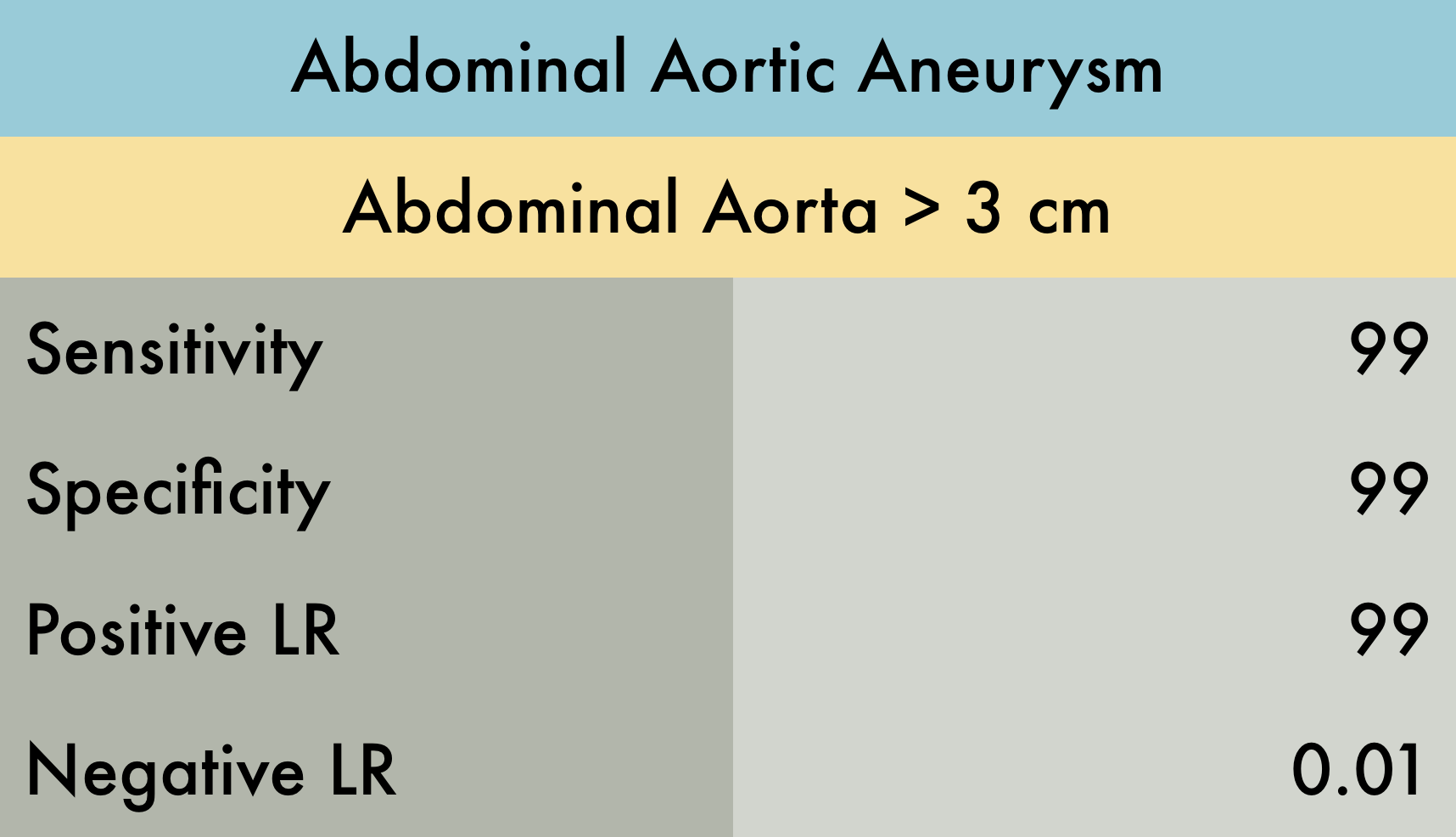
Abdominal Aortic Aneurysm
This was a systematic review evaluating the operating characteristics of emergency department (ED) performed ultrasonography for abdominal aortic aneurysm (AAA). A total of 7 studies (n = 655) were included in the analysis, all of which were prospective studies which enrolled adult patients with symptoms/signs suggestive of AAA. AAA was defined as > 3 cm dilation of the aorta. The reference standard was varied among studies including CT, MRI, aortography, radiology performed ultrasound, exploratory laparotomy, or autopsy results. The operator training and experience, as well as the number of participating emergency physicians in each study, was also quite variable. While the pooled data is displayed in the included table, the individual sensitivity and specificity range for AAA detection among the 7 studies were as follows: sensitivity 97.5-100%, specificity 94.1-100%, LR+ 10.8 - infinite, and LR- 0.00-0.025.
PMID: 23406071
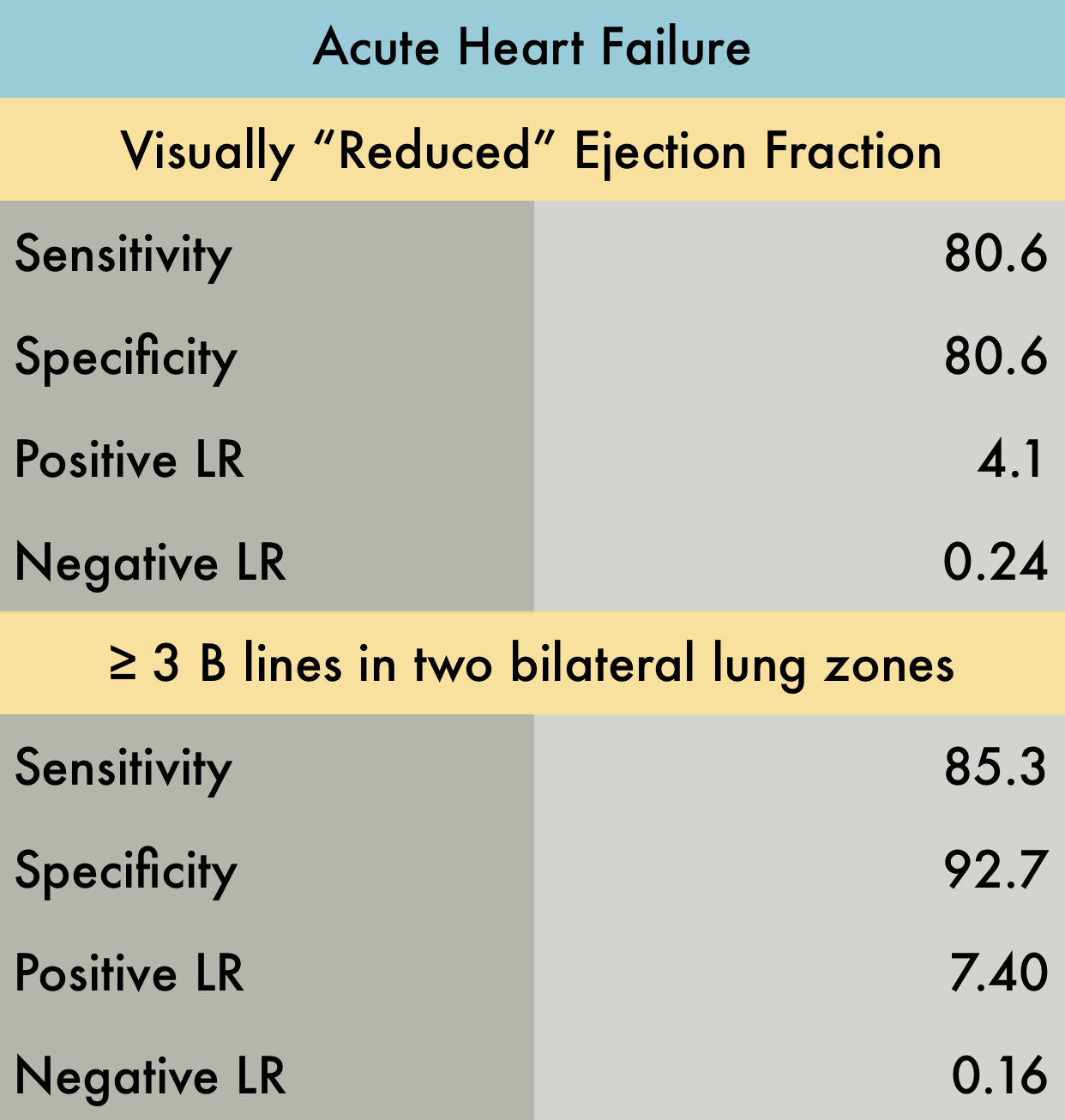
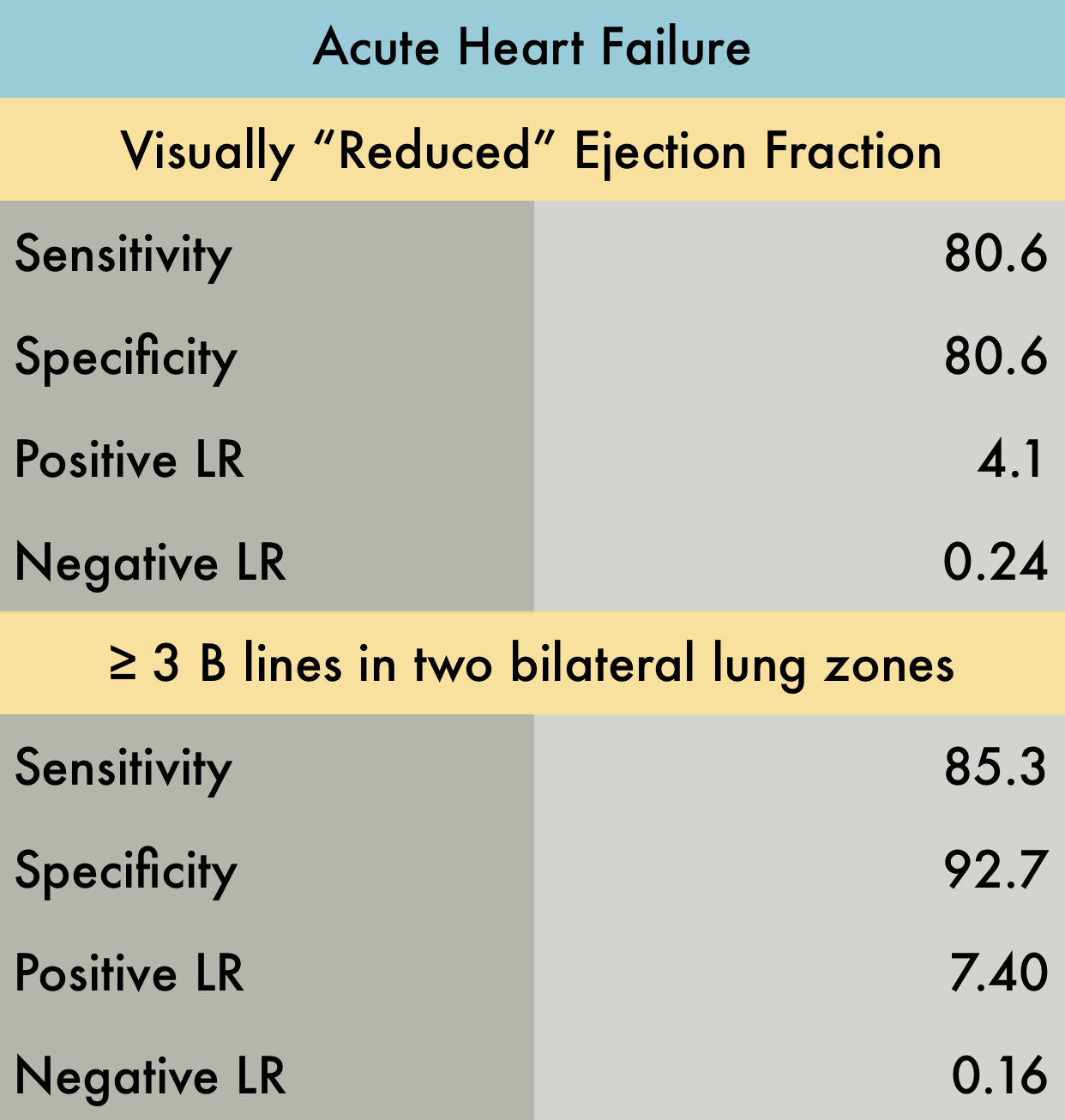
Acute Heart Failure
This was a large systematic review and meta-analysis (57 studies, n = 17,893) of the operating characteristics for diagnostic elements available to the emergency physician for diagnosing acute heart failure (AHF) including the history and physical, ECG, chest radiography, BNP/NT-proBNP (NPs), bedside echocardiography, lung ultrasound, and bioimpedance. They concluded that bedside lung US and echocardiography appear to the most useful tests for affirming the presence of AHF while NPs are valuable in excluding the diagnosis. Reduced ejection fraction was determined to have the highest +LR compared to other elements of the exam. However, the studied included in the final pooling appear to have only used "visual estimation" of reduced EF. With regards to lung US, a positive finding was defined in every study by the presence of at least three B lines in two bilateral lung zones.
PMID: 26910112
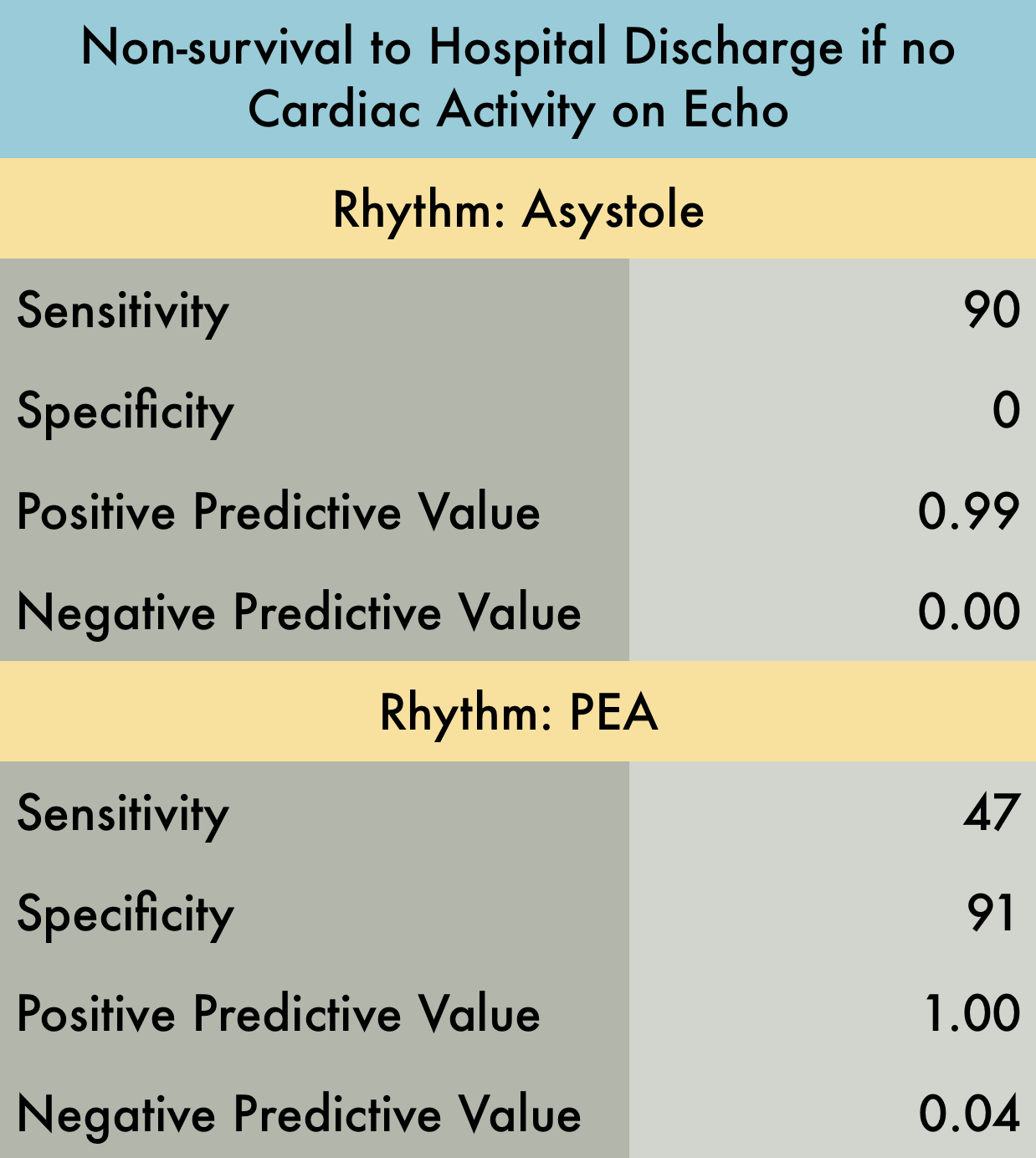
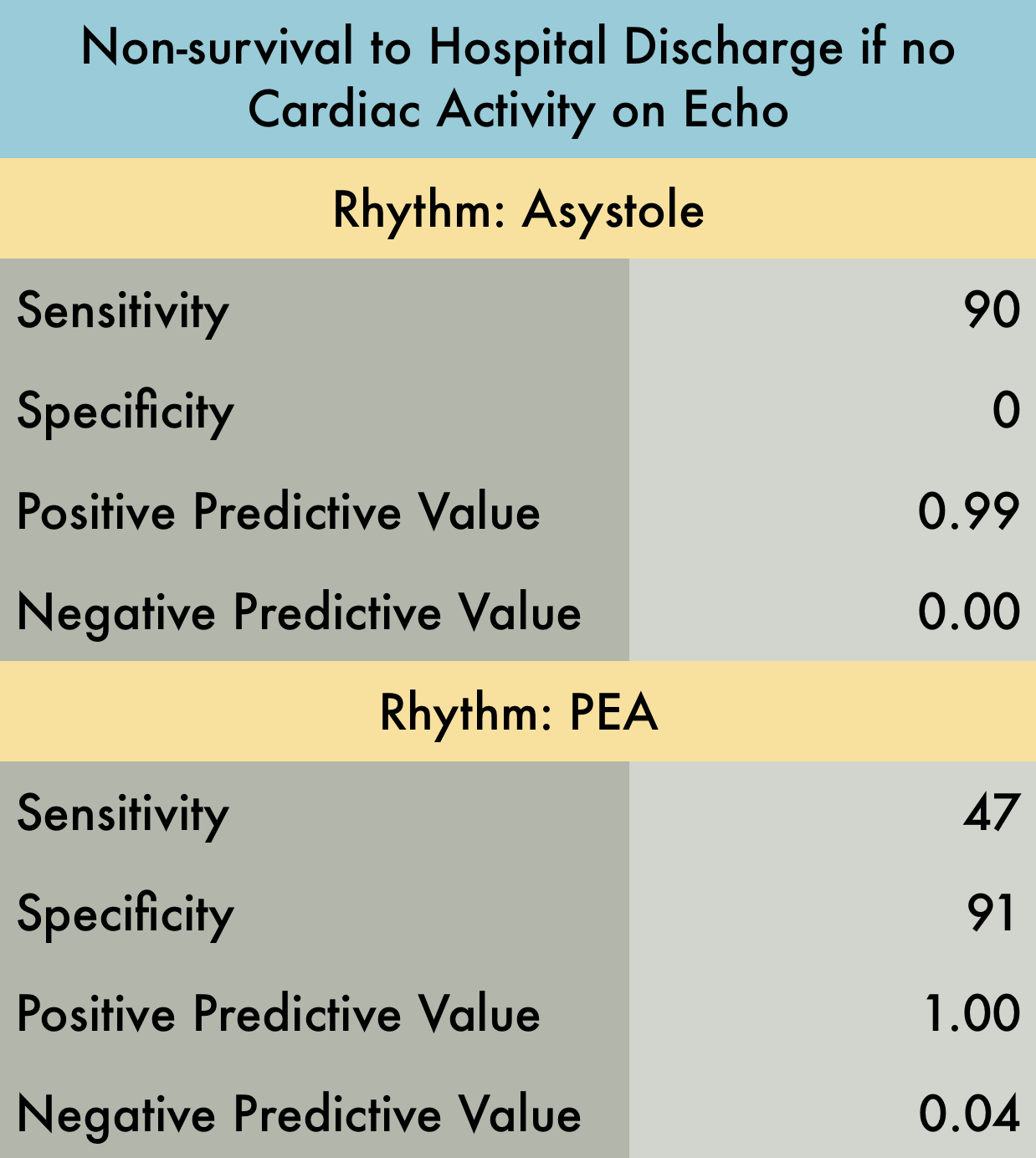
Cardiac Arrest Survival
This was a prospective observational study at 20 hospitals in the US and Canada evaluating patients presenting with out-of-hospital arrest or in-ED arrest. Patients with pulseless electrical activity or asystole were included. An ultrasound was performed at the beginning and end of ACLS. Clinicians were not blinded to the ultrasound results. Patients with short resuscitation time ( < 5 minutes) were excluded to avoid including patients with resuscitation efforts stopped because of a negative ultrasound. Their findings demonstrated that patients in asystole without cardiac activity are unlikely to benefit from prolonged resuscitation as survival rate is dismal. Note that Positive Predictive Value was used in provided table as this is easier to interpret with respect to their data. Positive predictive value is the probability that subjects with a positive screening test truly have the disease. With respect to the study data, positive predictive value represents the probability that a patient WILL NOT survive if they have no cardiac activity on bedside echo and are in asystole (or PEA).
PMID: 27693280
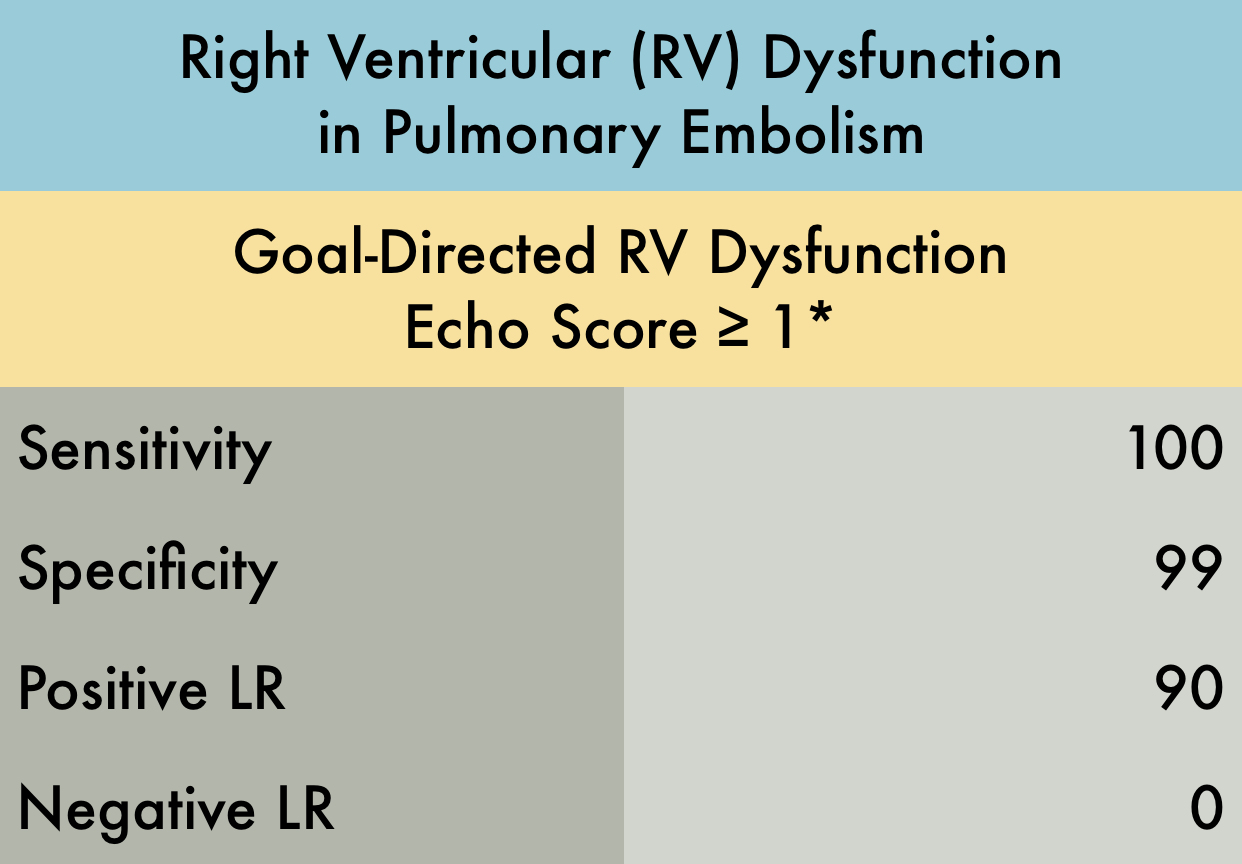
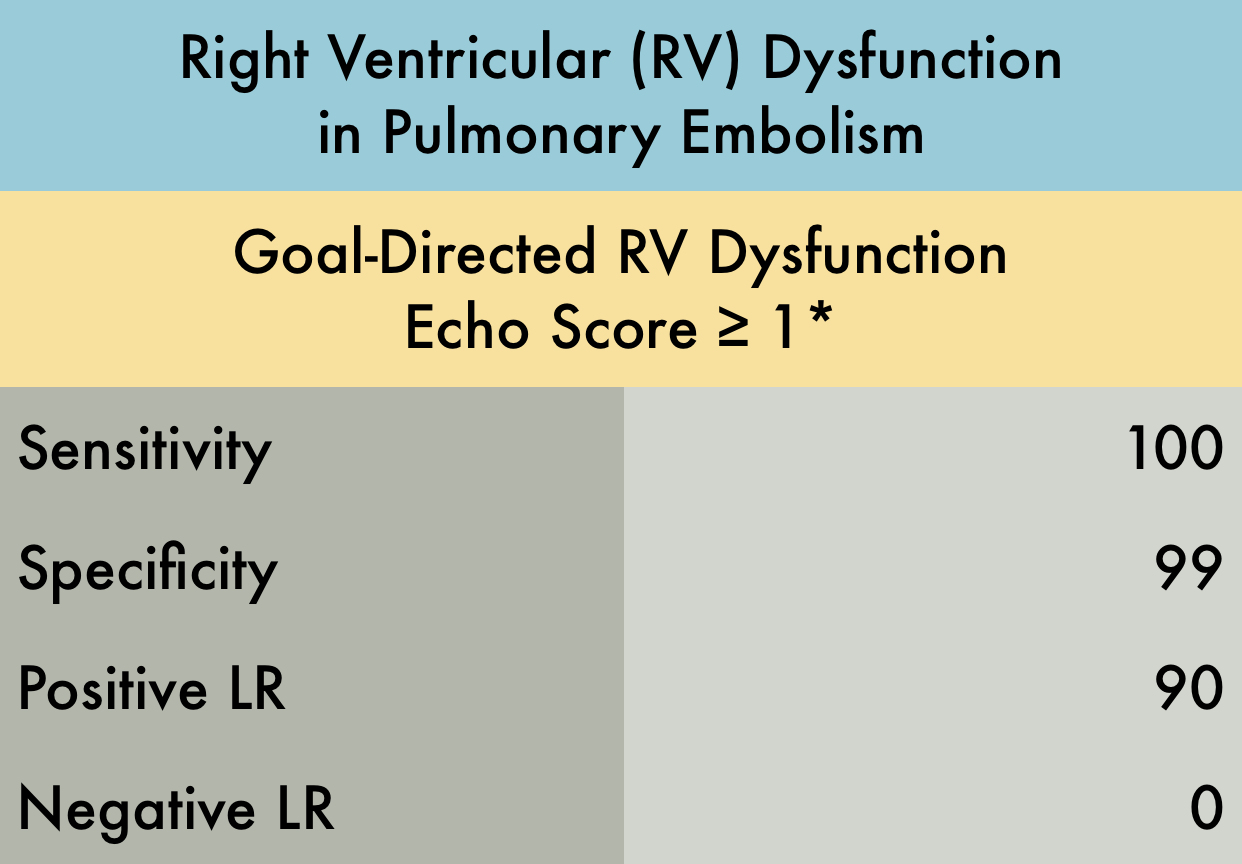
Right Ventricular Dysfunction in PE
This was a prospective observational study (n=116) of consecutive normotensive patients with confirmed pulmonary embolism, assessing the diagnostic accuracy of biomarkers, CT, and goal-directed echocardiography for right ventricular dysfunction. Emergency physicians, blinded to clot burden and biomarkers, performed qualitative goal-directed echocardiography for right ventricular (RV) dysfunction*: RV enlargement (RV diameter greater than or equal to that of the left ventricle), severe RV systolic dysfunction (RV free wall hypokinesis or TAPSE < 1.0 cm), and/or interventricular septum flattening or bowing into the left ventricle. If any one of these were present, right ventricular dysfunction was diagnosed. Goal-directed echocardiography results were compared to comprehensive echocardiography as the gold-standard.
PMID: 26973178
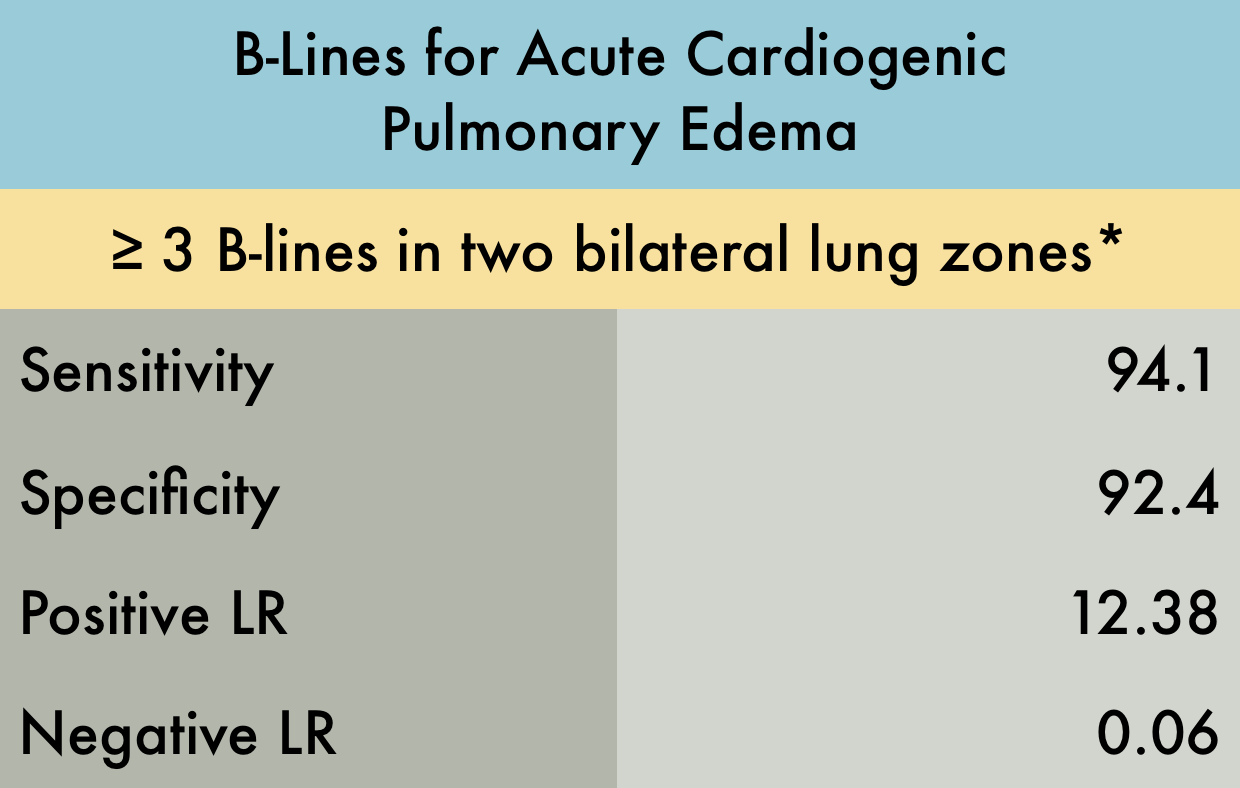
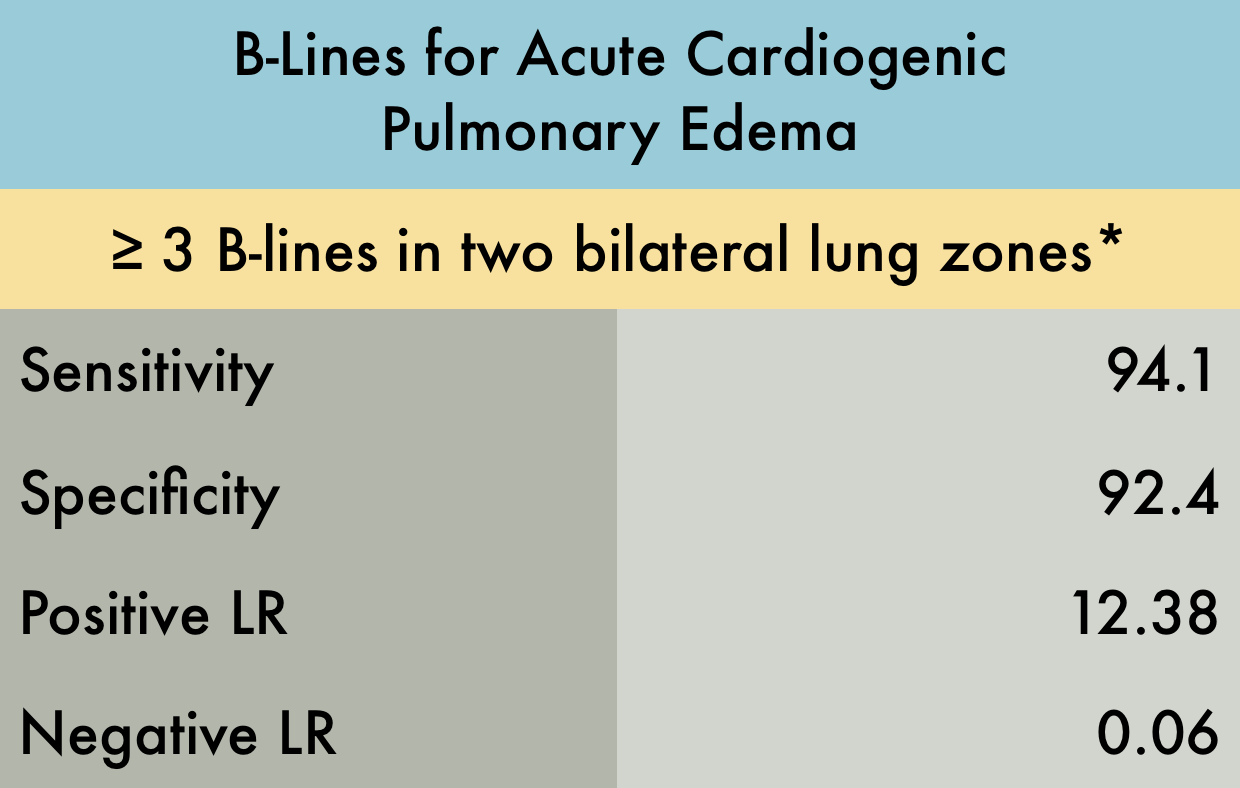
Pulmonary Edema in Heart Failure
This was a systematic review including 7 prospective case control or cohort studies (n=1075) evaluating the sensitivity and specificity of B-lines in diagnosing acute cardiogenic pulmonary edema (ACPE). The included studies recruited patients presenting to the hospital with acute dyspnea, or where there was a clinical suspicion of congestive heart failure. The setting was either the emergency department (ED) , ICU, or inpatient wards. Ultrasound examinations were performed by any non-radiologist physician. *Various lung ultrasound protocols were used, including the Volpicelli method, the Lichtenstein protocol, and the Comet Score. All involved using B-lines to make the diagnosis of ACPE. The varied protocols used for diagnosis may explain the increased sensitivity noted in this study compared to other meta-analysis. Gold standard was heterogeneous amongst studies with 'final diagnosis from clinical follow-up' being an acceptable reference standard.
PMID: 25176151
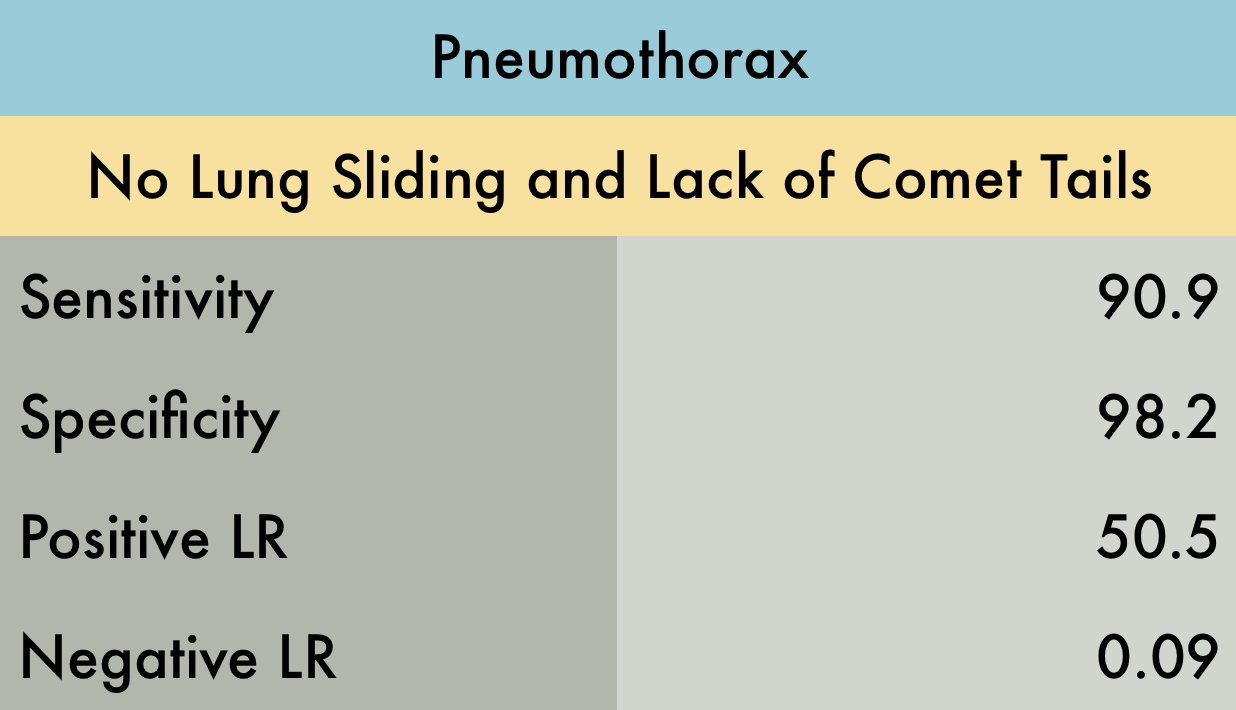
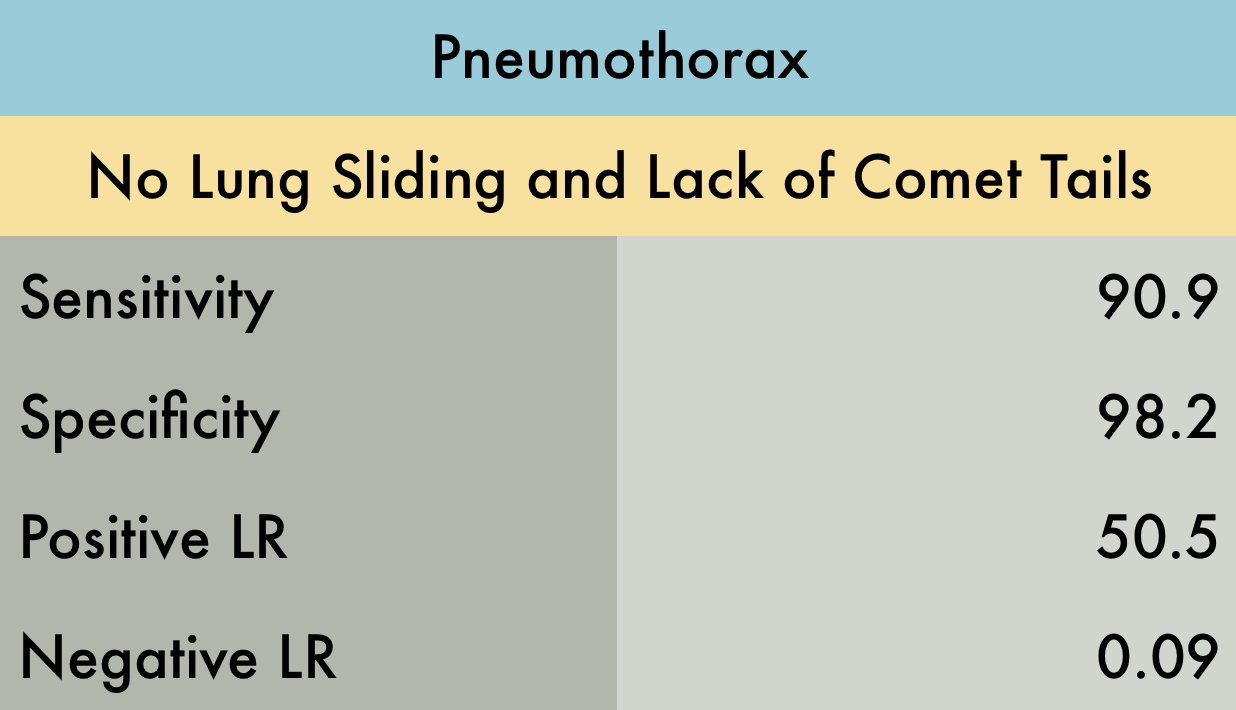
Pneumothorax
This was a systematic review of 8 prospective studies (n=1048) of adult patients. Included manuscripts evaluated for traumatic or iatrogenic pneumothorax. No studies that screened for spontaneous pneumothorax were included. Examiners were surgeons, radiologists, or emergency providers. Reference standard was pneumothorax found on CT or a rush of air upon tube thoracostomy. All studies but one used the ultrasonographic signs of lung sliding and comet tail to rule out pneumothorax. Although the exact technique used to perform the ultrasound examination is not reported with enough detail in some studies, most agree on requiring the examination of more than one intercostal space in both the midclavicular line and laterally and inferiorly at the anterior or midaxillary lines. Lastly, this data does not evaluate whether the pneumothoraces identified were clinically significant.
PMID: 21868468
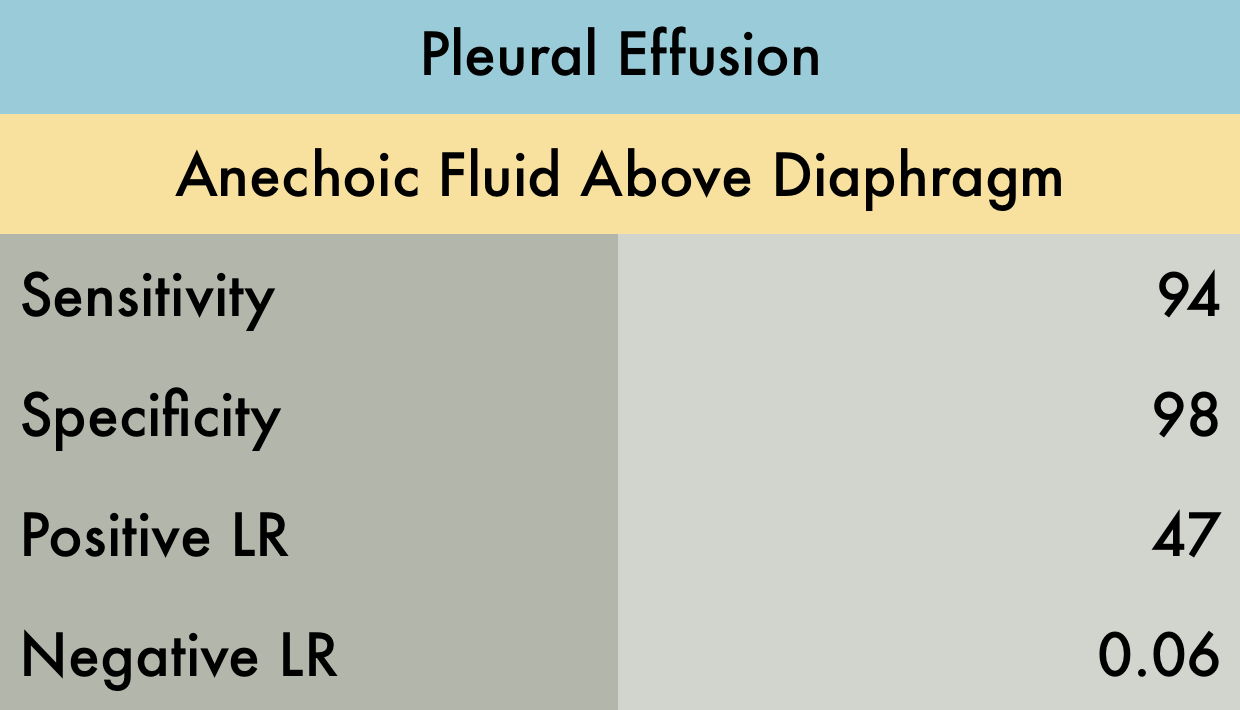
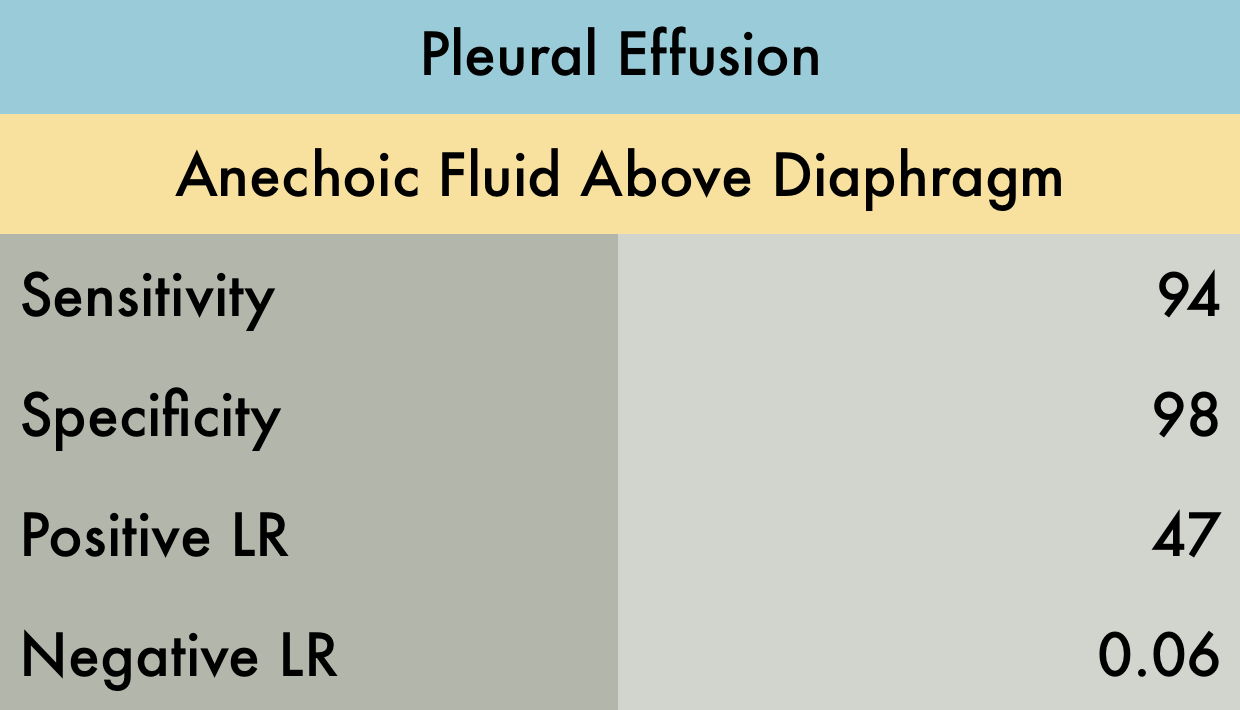
Pleural Effusion
This was a meta-analysis including 12 retrospective and prospective studies (n=1554) of adults and pediatric patients. Ultrasound was used to diagnose pleural effusion, with the reference standard either CT, surgery, or a more formal “high quality ultrasound in conjunction with expert end diagnosis.” Ultrasound examinations were performed by a variety of operators including emergency physicians, intensivists, radiologists, and nurses. Exact criteria for diagnosis of a pleural effusion by ultrasound was not defined.
PMID: 26862542
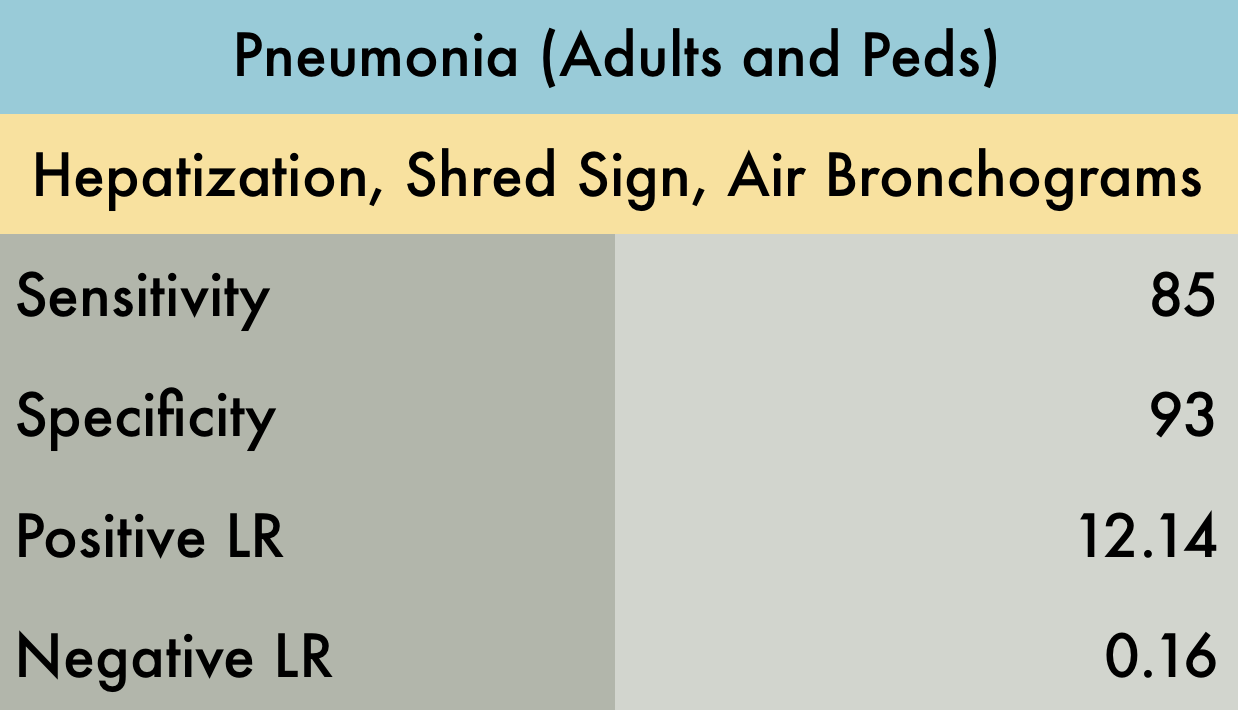
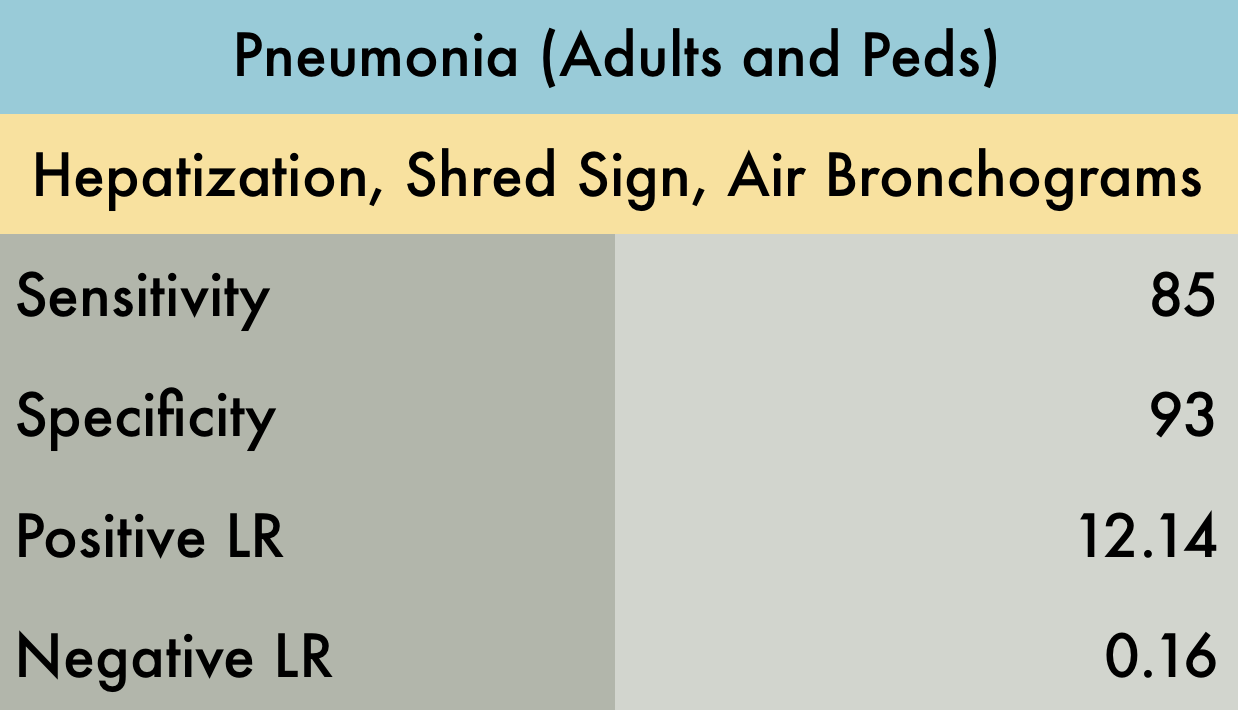
Pneumonia (Adults and Peds)
The was a systematic review including 20 prospective adult and pediatric studies (n=2513) with varied settings including the emergency department, inpatient wards, or ICU. A positive finding on ultrasound was identified as an alveolar and interstitial pattern or consolidation, although this is not further expanded upon. Gold standard was either CT, chest radiography, or “clinical diagnosis” depending on the study. One large caveat of this study is that it has a very large degree of heterogeneity, with ultrasound examinations performed by emergency physicians, intensivists, and radiologists of varying levels of expertise, on patients ranging from ambulatory to critically ill.
PMID: 28244009
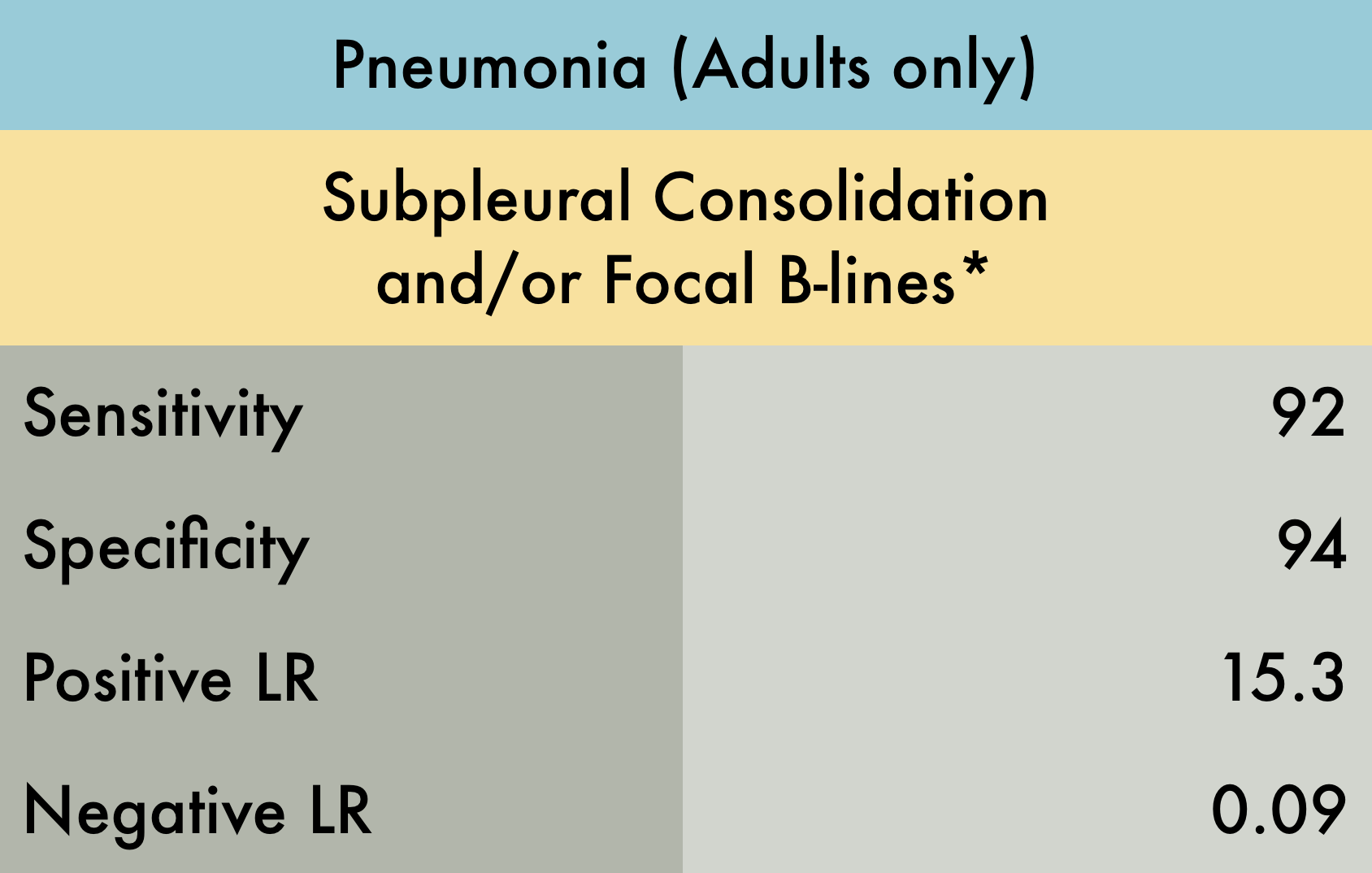
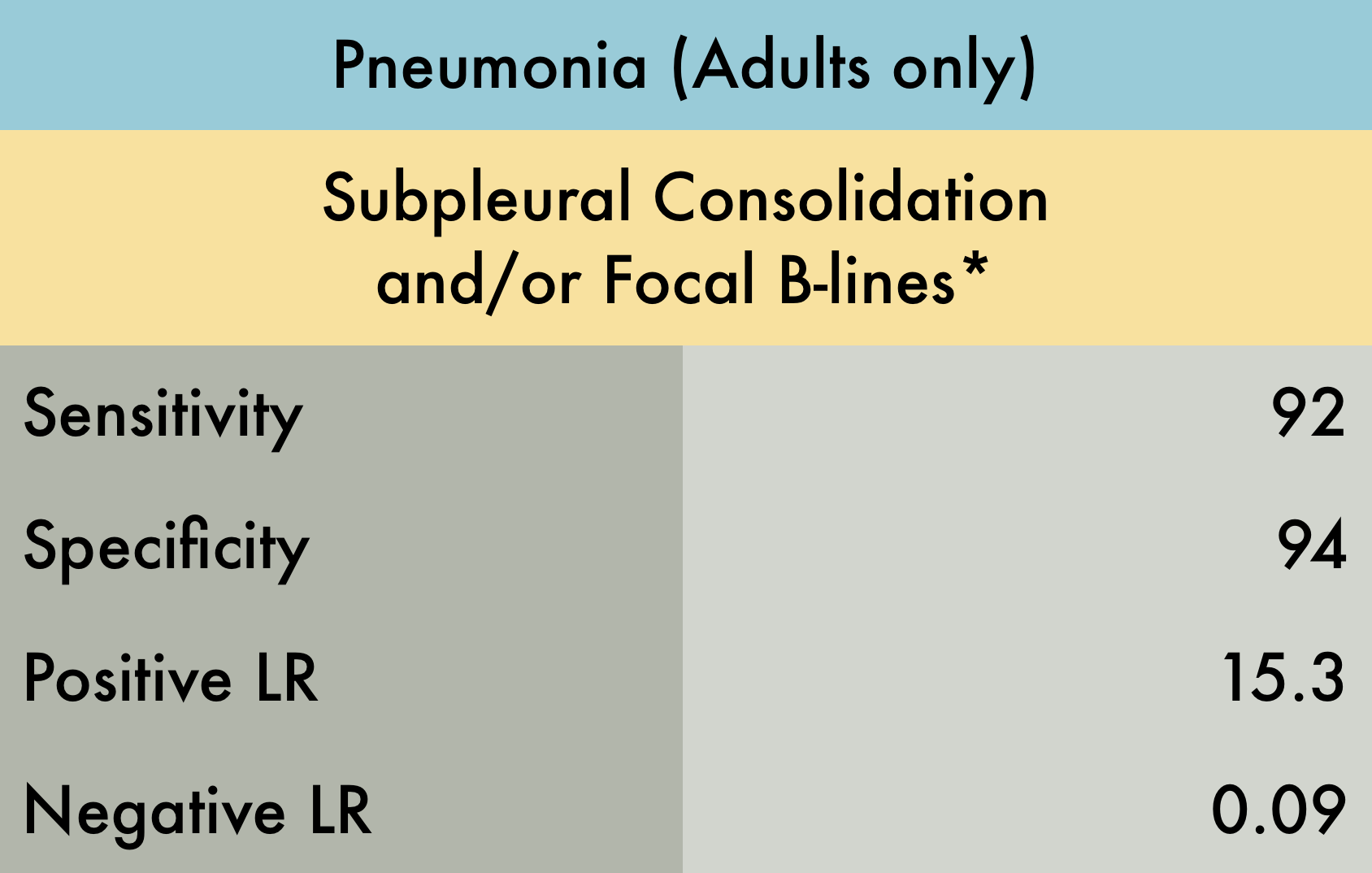
Pneumonia (Adults only)
This was a systematic review including 17 prospective studies (n=5108) evaluating the operating characteristics of lung ultrasound for pneumonia in adult patients seen in the emergency department with a clinical suspicion for this diagnosis. Reference standard was either chest radiograph, chest CT, or final clinical diagnosis. Included studies varied with regards to which and how many lung fields were evaluated. The operators performing ultrasound examinations were exclusively emergency physicians or radiologists.*Subpleural consolidation and/or focal B-lines were the diagnostic criteria in the majority of manuscripts included, however in 4 studies, no clear positive findings were specified.
PMID: 29189351
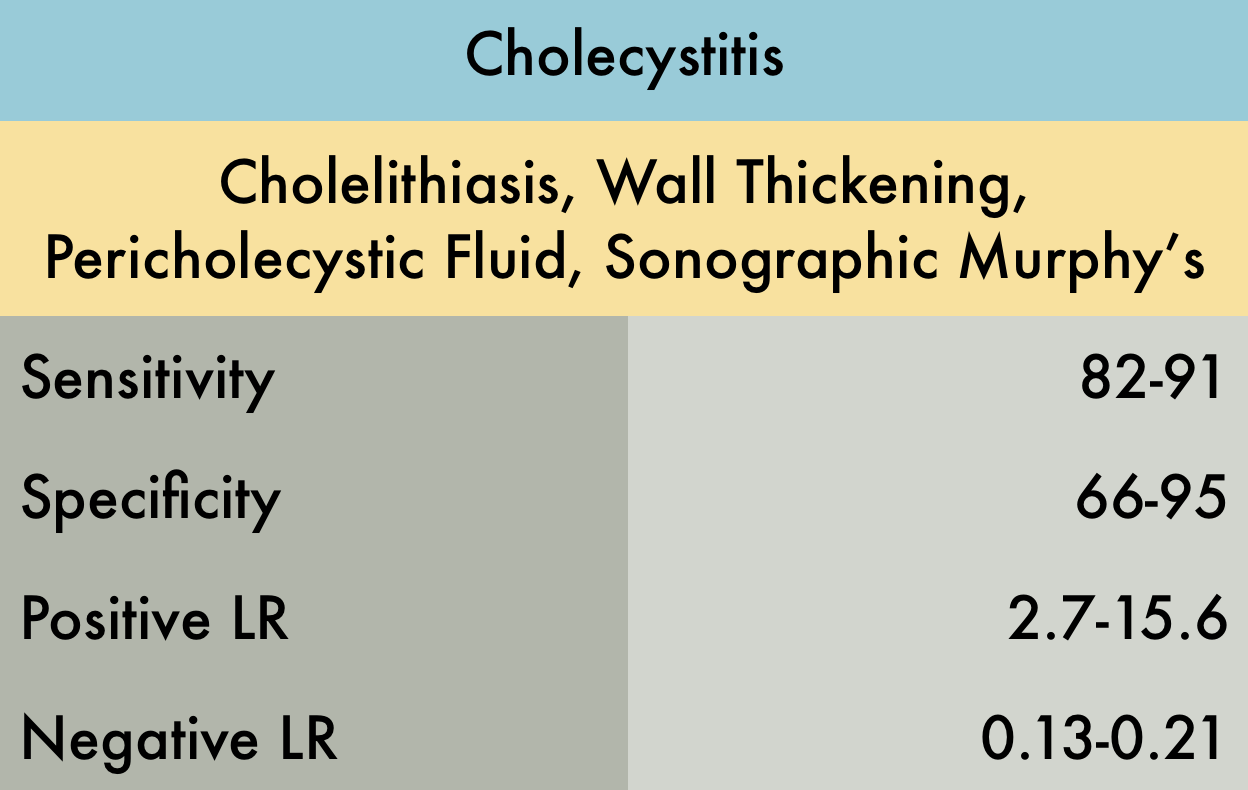
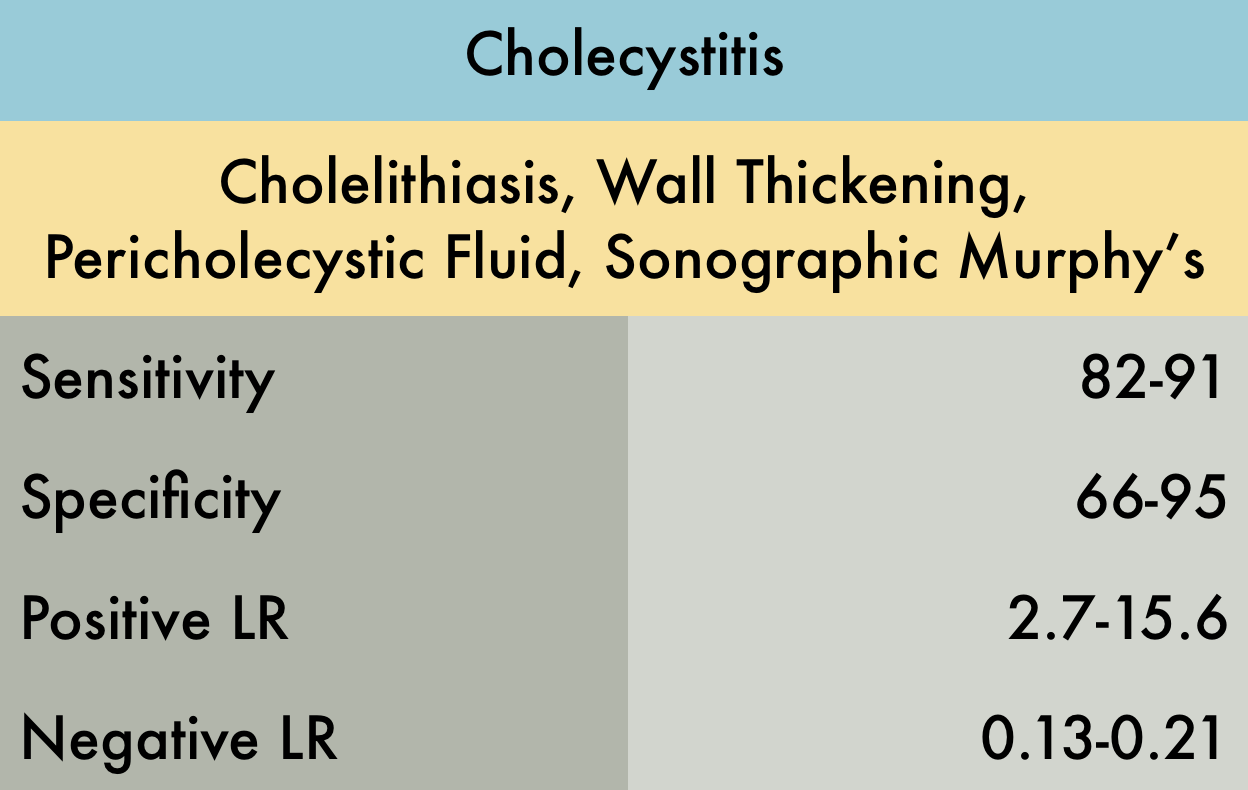
Cholecystitis
This was a systematic review including 4 prospective studies evaluating the operating characteristics of bedside ultrasound for acute cholecystitis (AC) in adult patients seen in the emergency department with a clinical suspicion for AC or right upper quadrant pain. Sample size of the studies varied from 30 to 193 subjects. Reference standard was surgical pathology. The experience of the sonographers varied between the studies and in one study no documentation of sonographer experience was noted. There was significant heterogeneity across the included studies precluding the authors ability to pool the results hence a range is noted in the operating characteristics table.
PMID: 27862628
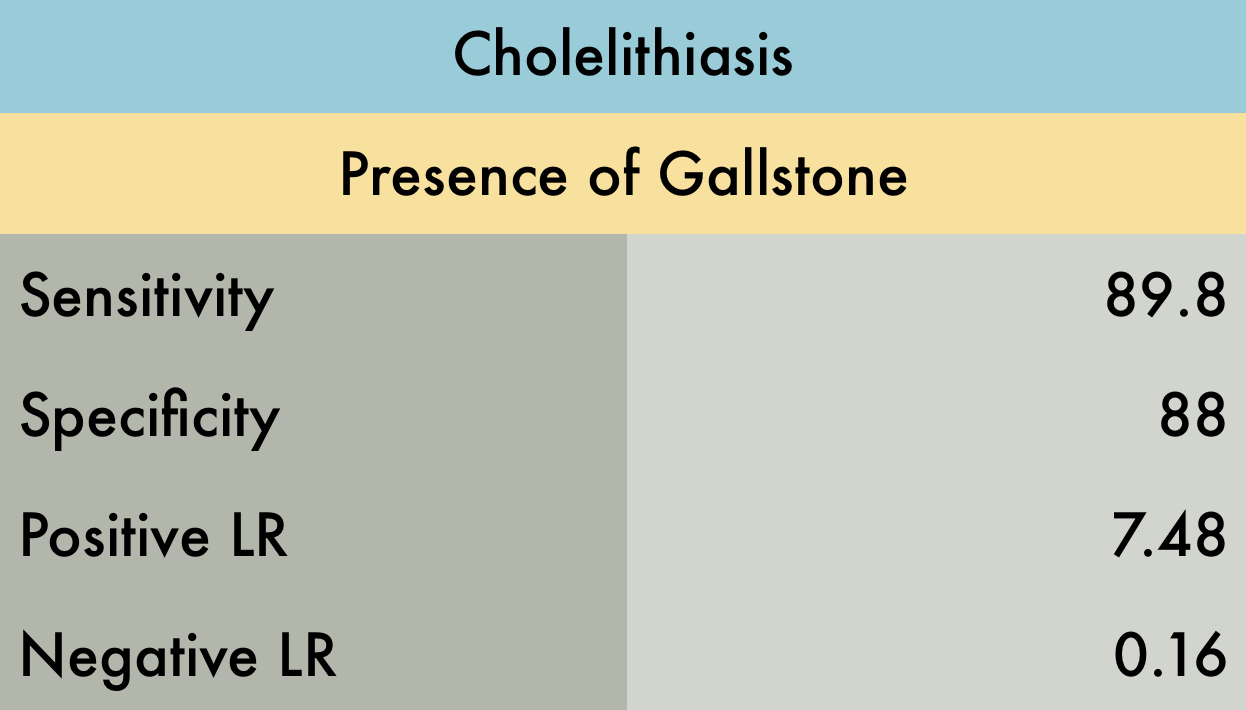
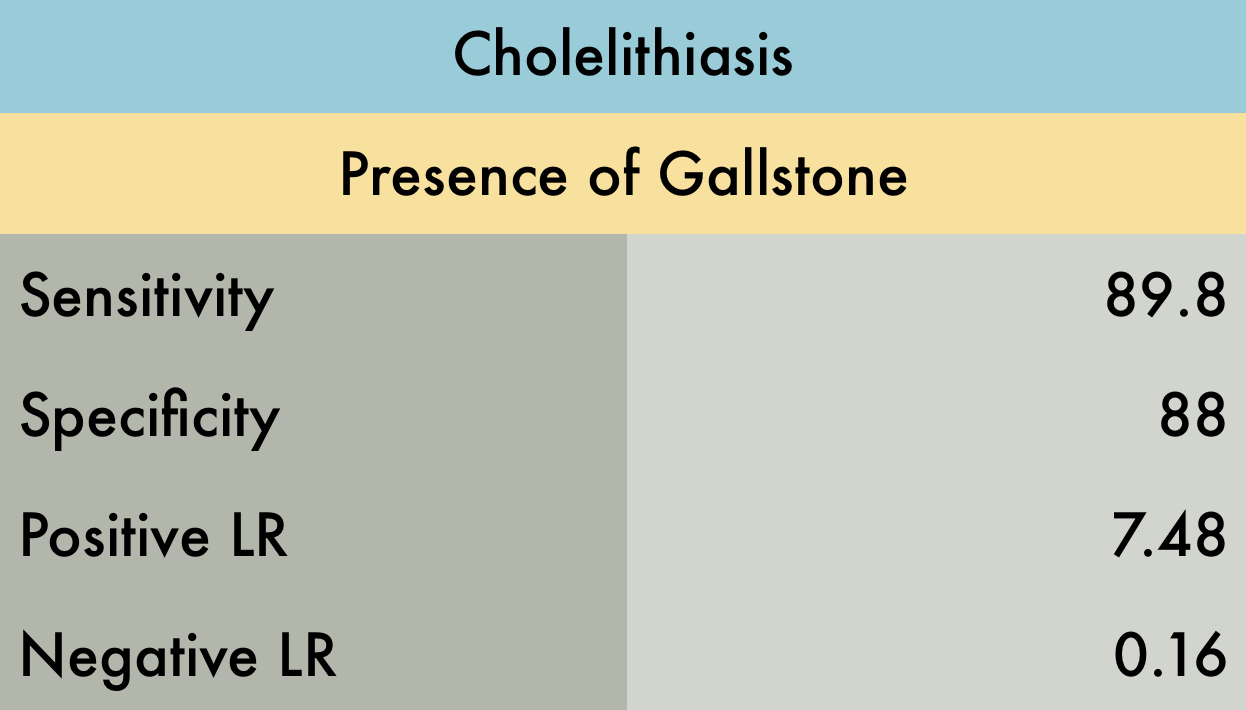
Cholelithiasis
This was a meta-analysis including 8 studies (n=710) evaluating the operating characteristics of emergency ultrasound (EUS) for identifying cholelithiasis in adult patients presenting to the emergency department with symptoms suggestive of biliary colic (RUQ pain, epigastric pain, or right flank pain). Reference standards included radiology performed ultrasound, CT, MRI, and/or surgical pathology. There was quite a variation in the technical ability between operators which may distort the pooled sensitivity and specificity.
PMID: 21401784
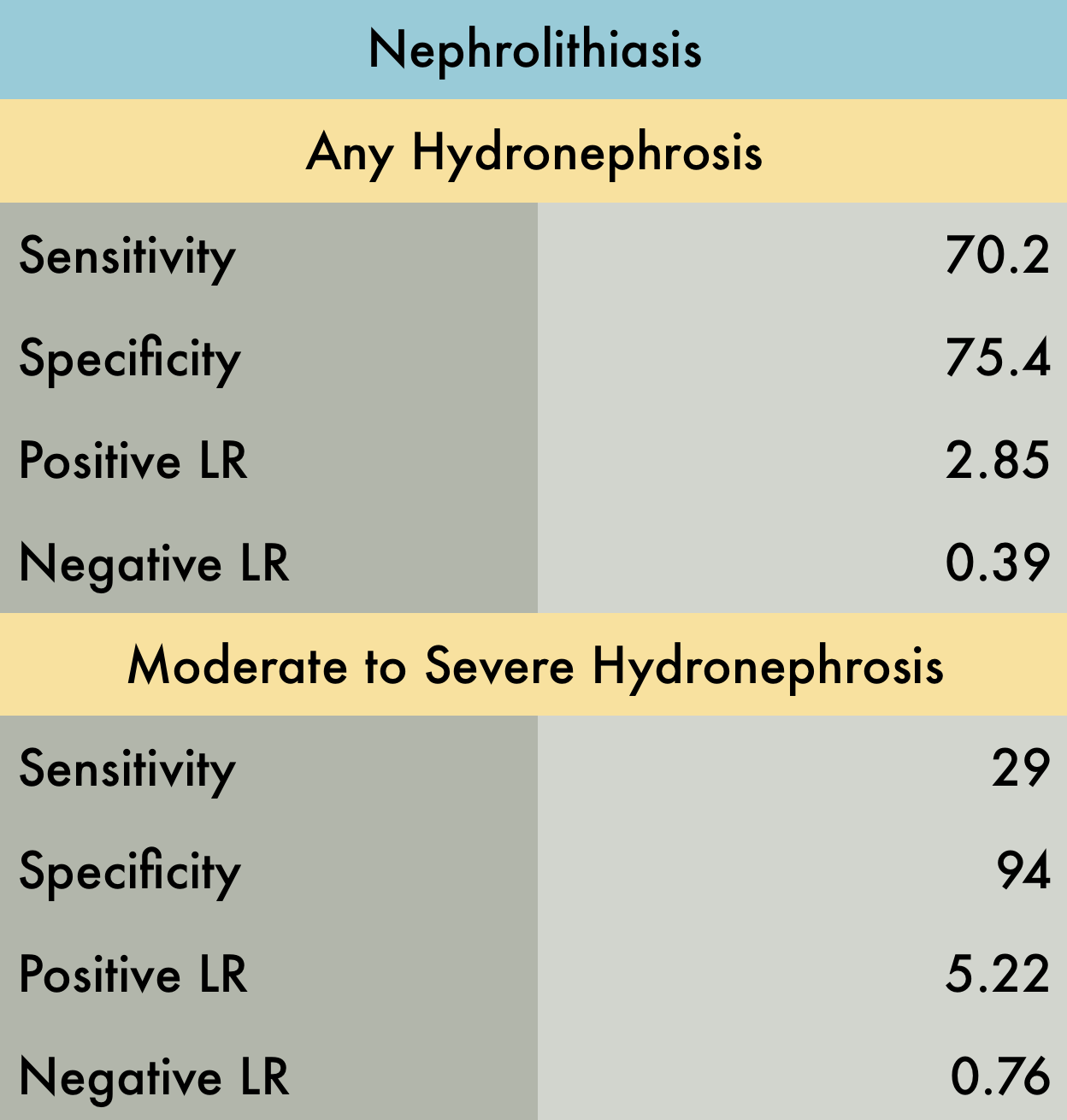
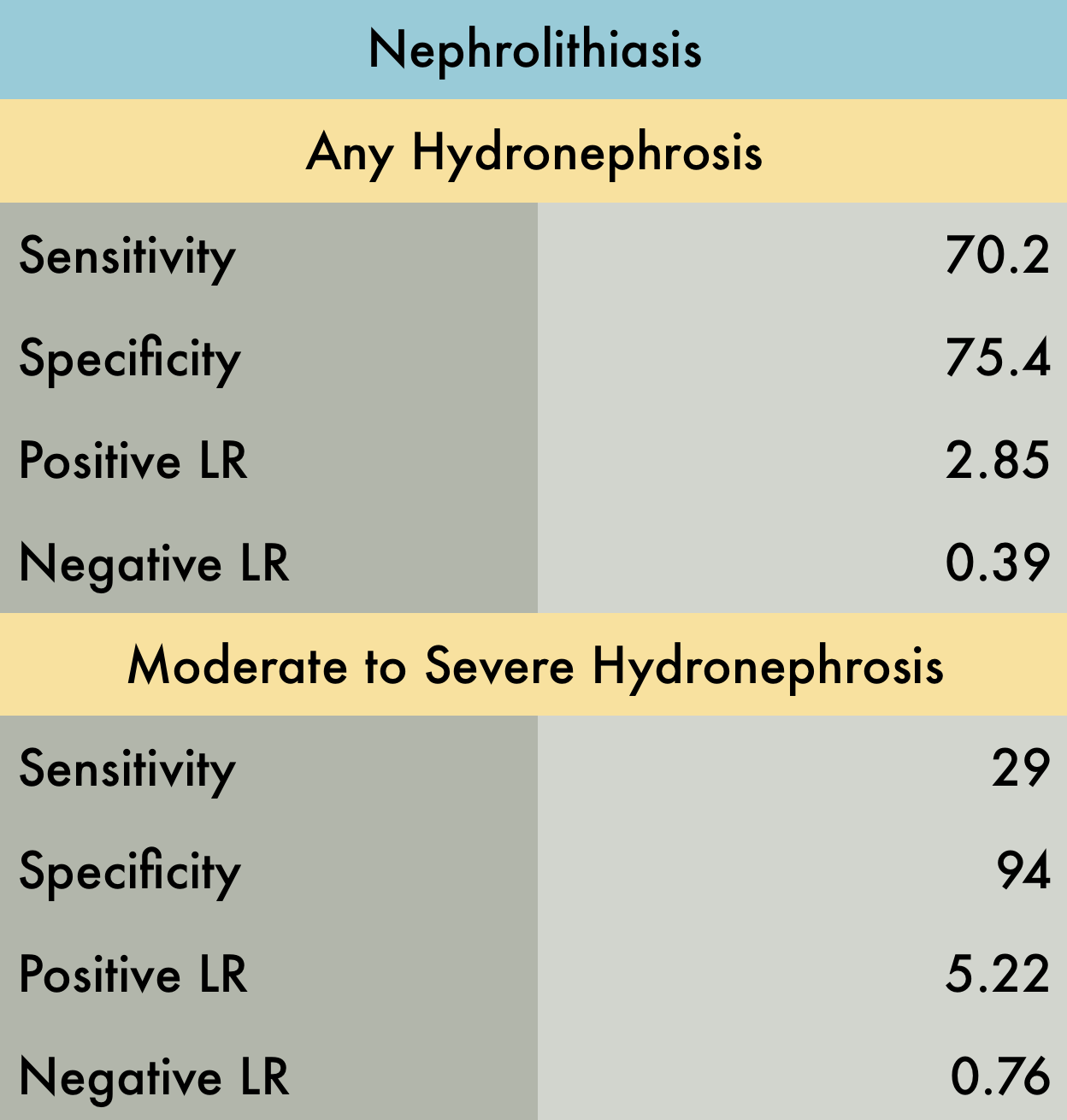
Nephrolithiasis
This was a meta-analysis including 5 studies (n=1773) evaluating the accuracy of POCUS to diagnose nephrolithiasis in adult patients presenting to the emergency department with symptoms suggestive of renal colic (flank pain, dysuria, abdominal pain radiating to groin). Reference standards included CT, direct stone visualization, or surgical findings. Specificity improved significantly (~94.4%) for moderate to severe hydronephrosis (i.e. exclusion of mild hydronephrosis). This systematic review has some flaws (most importantly not having a single uniform gold standard) but appears to be the best available evidence.
PMID: 29427476
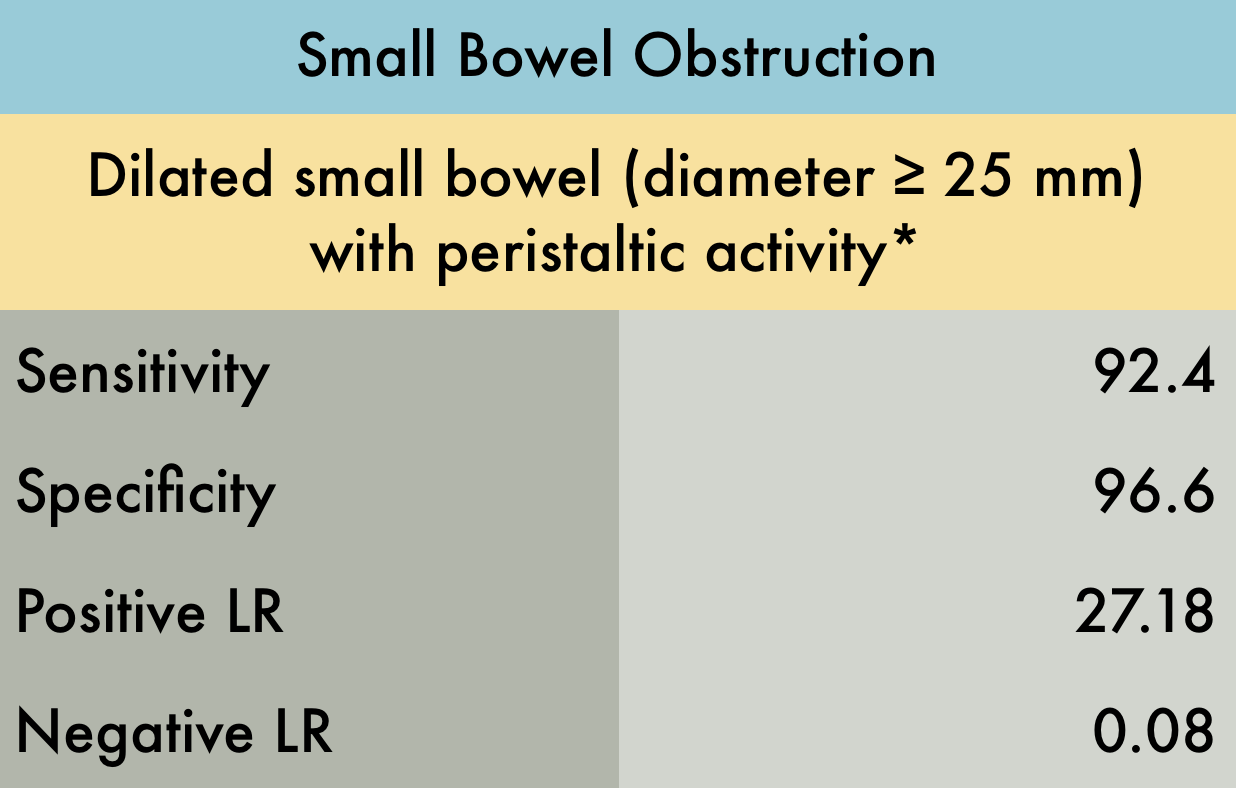
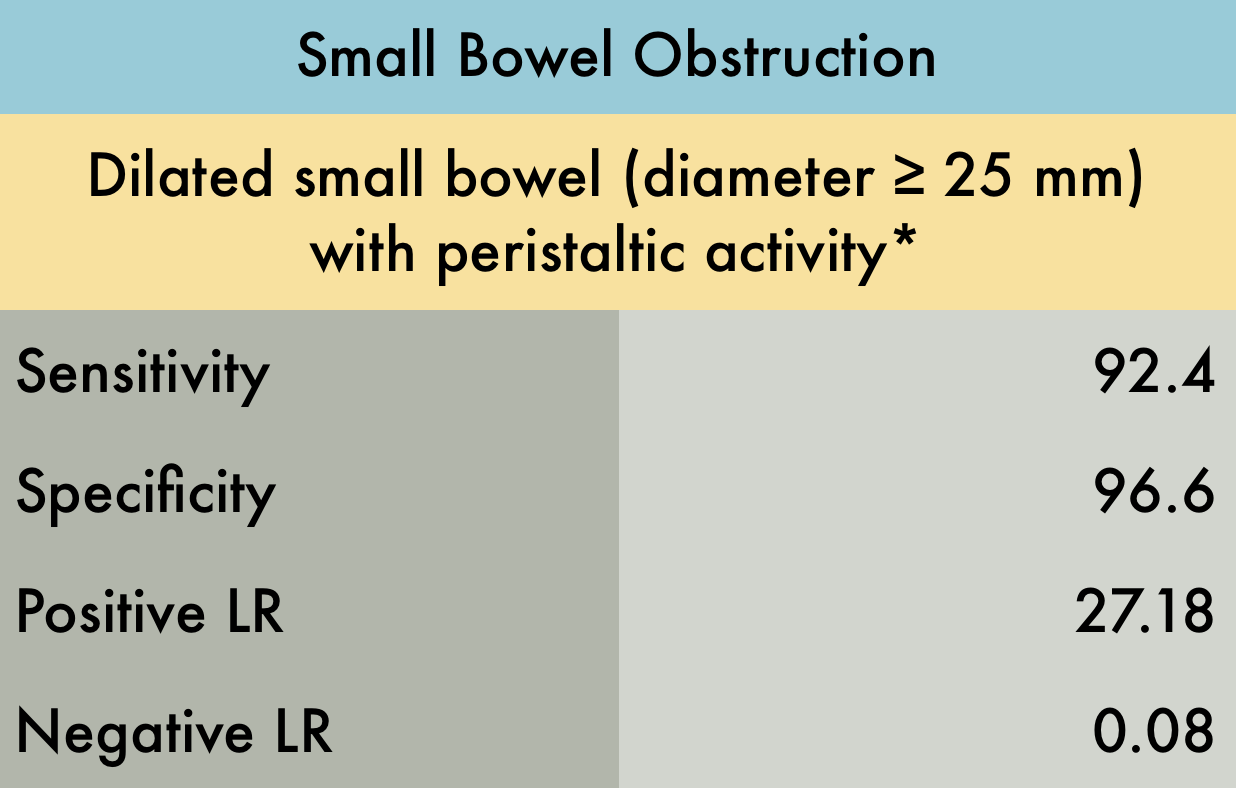
Small Bowel Obstruction
This was a meta-analysis including 11 studies (n=1178) to evaluate the test characteristics of US in diagnosis of small bowel obstruction (SBO). There was mild to moderate heterogeneity in diagnostic criteria, study location, sonographer experience, and reference standard. Specifically, most studies used 2.5 cm as the cutoff to diagnose SBO while one study used the cutoff of 3.0 cm, and several other studies only noted the presence of “dilated bowel loops” as a diagnostic criteria. Of the 11 studies included, only 3 were emergency department studies. Reference standards included surgery, clinical diagnosis, CT, or other advanced imaging. While there were multiple components to the index test and varied reference standard, this does appear to be the best and biggest review on this topic. These operating characteristics suggest ultrasound to be a valuable tool in the diagnosis of SBO, however further studies are needed specifically with regards to the emergency department setting. *Other diagnostic criteria included visualizing collapsed distal loops of bowel with decreased peristalsis
PMID: 28797559
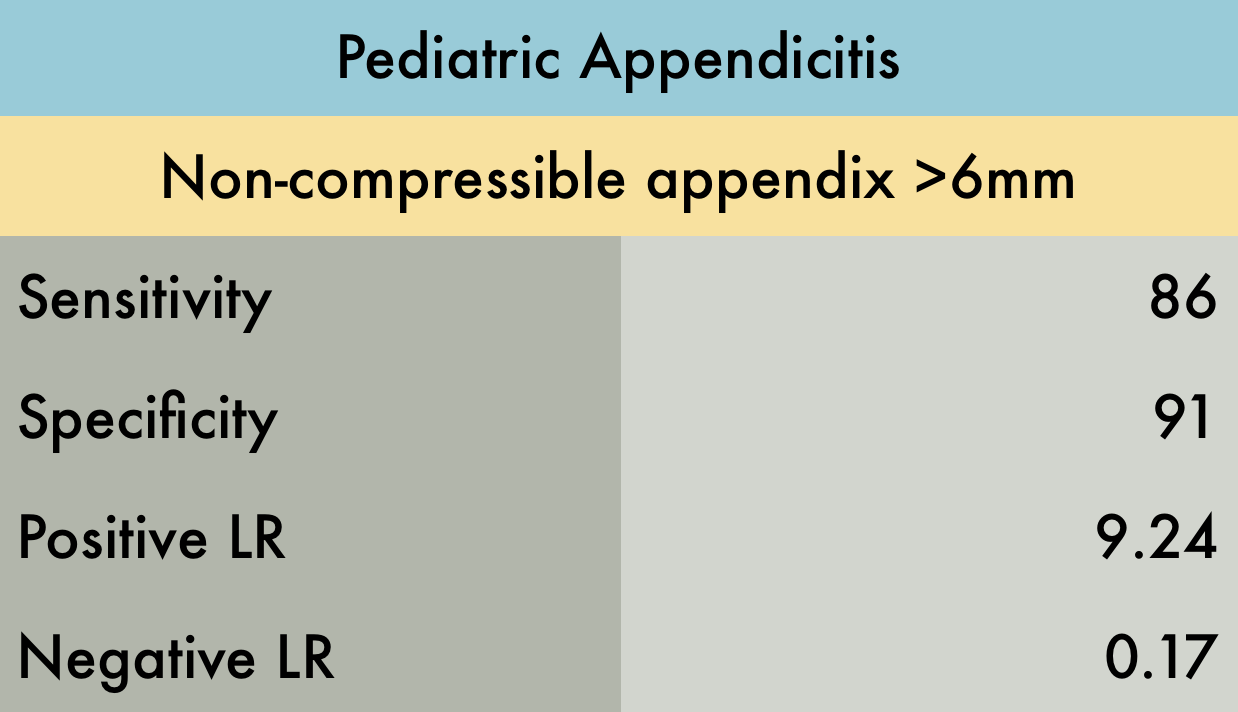
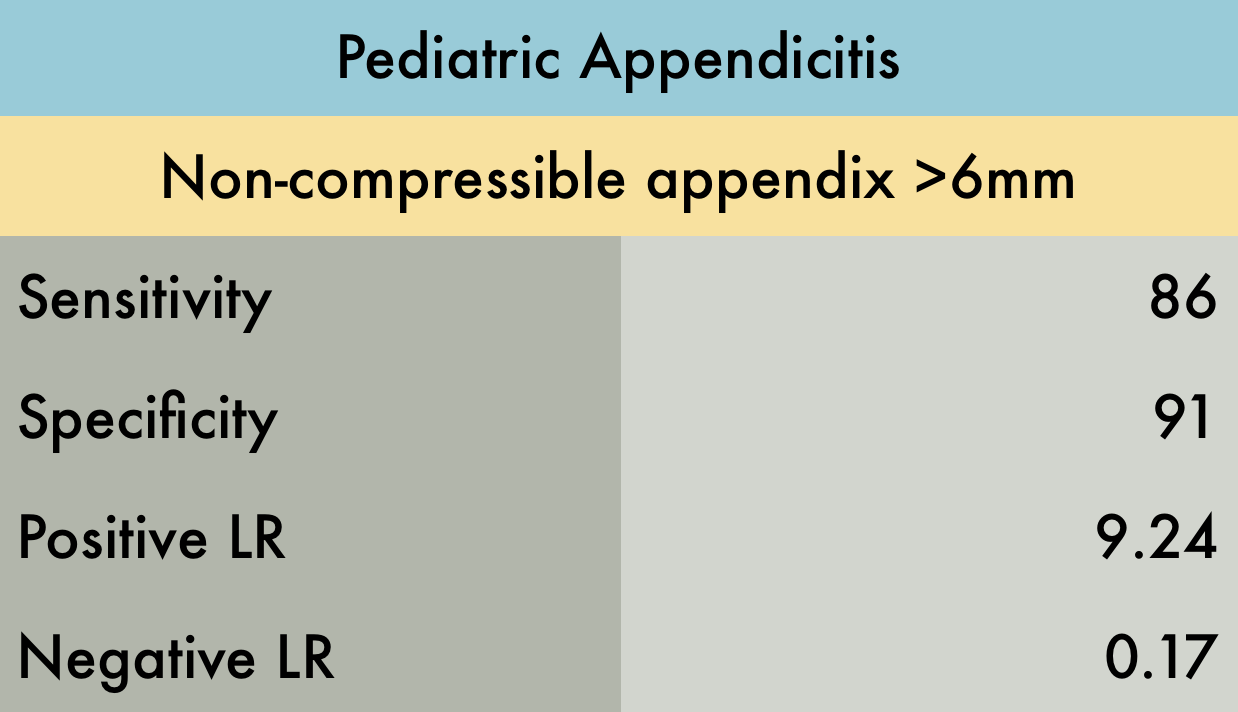
Pediatric Appendicitis
This systematic review and meta-analysis of 4 studies (n=461) evaluated the accuracy of emergency department POCUS performed by EM or PEM physicians for diagnosis of acute appendicitis in children. The main limitation of the study was the high prevalence of equivocal results. However, authors did a sensitivity analysis with and without equivocal cases and results were similar. A mathematical model was used to compare POCUS to CT scan and MRI. The authors concluded that a positive POCUS exam is diagnostic, obviating the need for CT, however if POCUS is equivocal or negative, further imaging with CT or MRI is necessary.
PMID: 28214369
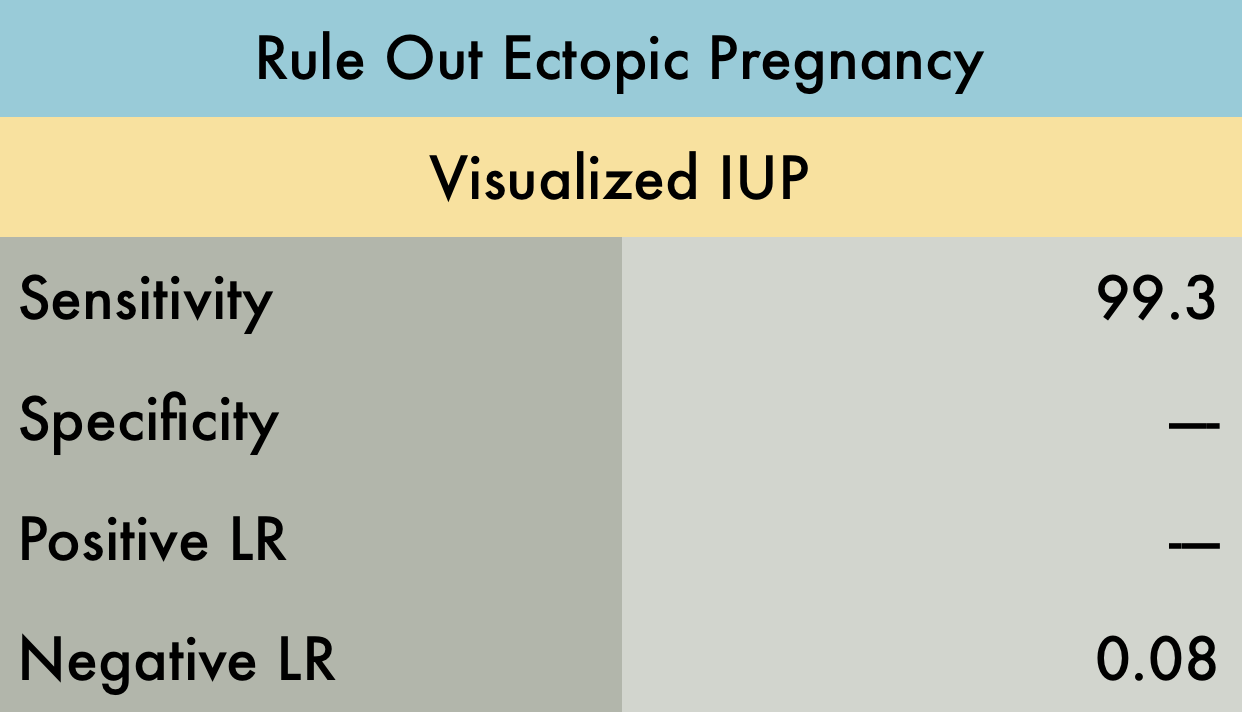
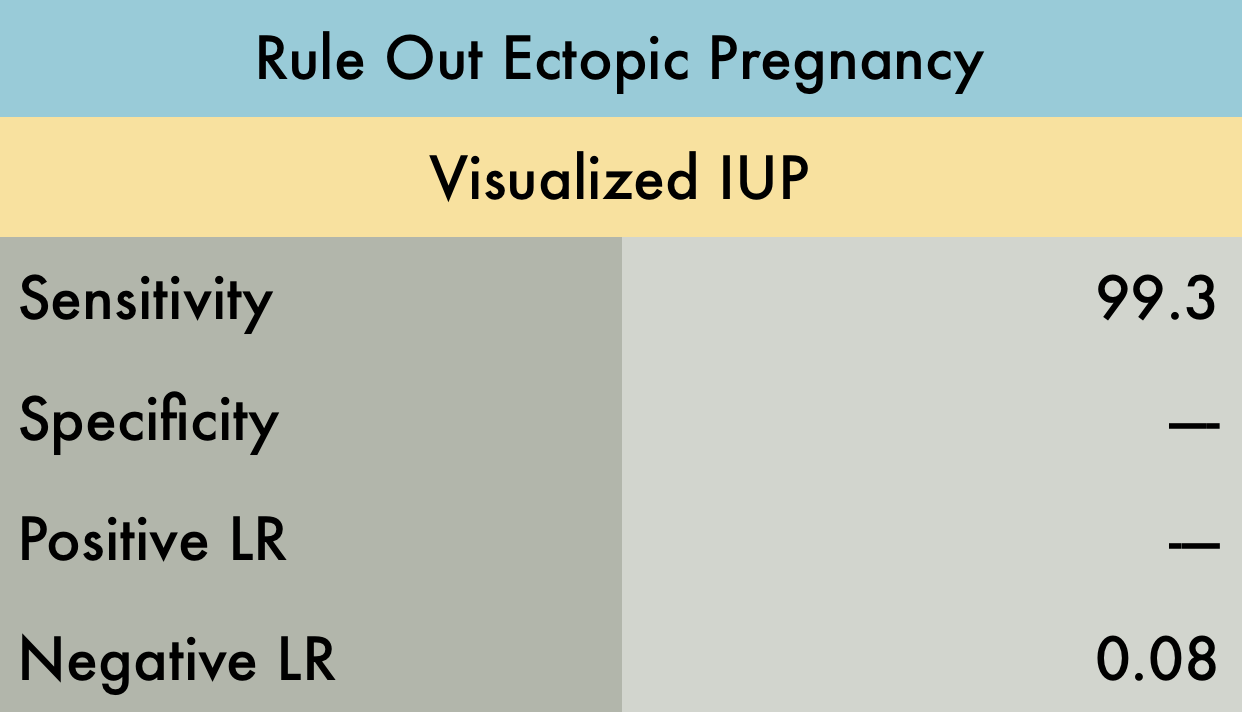
Ectopic Pregnancy
This was a meta-analysis including 10 studies (n=2057) examining the operating characteristics of bedside emergency provider (EP) performed ultrasound to rule out ectopic pregnancy. All studies used the visualization of an IUP (intrauterine pregnancy) on ultrasound as the rule out criteria. The ultrasound examinations performed by EPs included transabdominal, transvaginal or both. Reference standards included formal radiology US, gynecology US, over-read of EP performed US by radiology, or clinical record review. They did not report specificity and positive LR's because of significant heterogeneity in these results when data was pooled. This study supports the utility of EP performed ultrasound as a strong rule out test for ectopic pregnancy.
PMID: 20828874
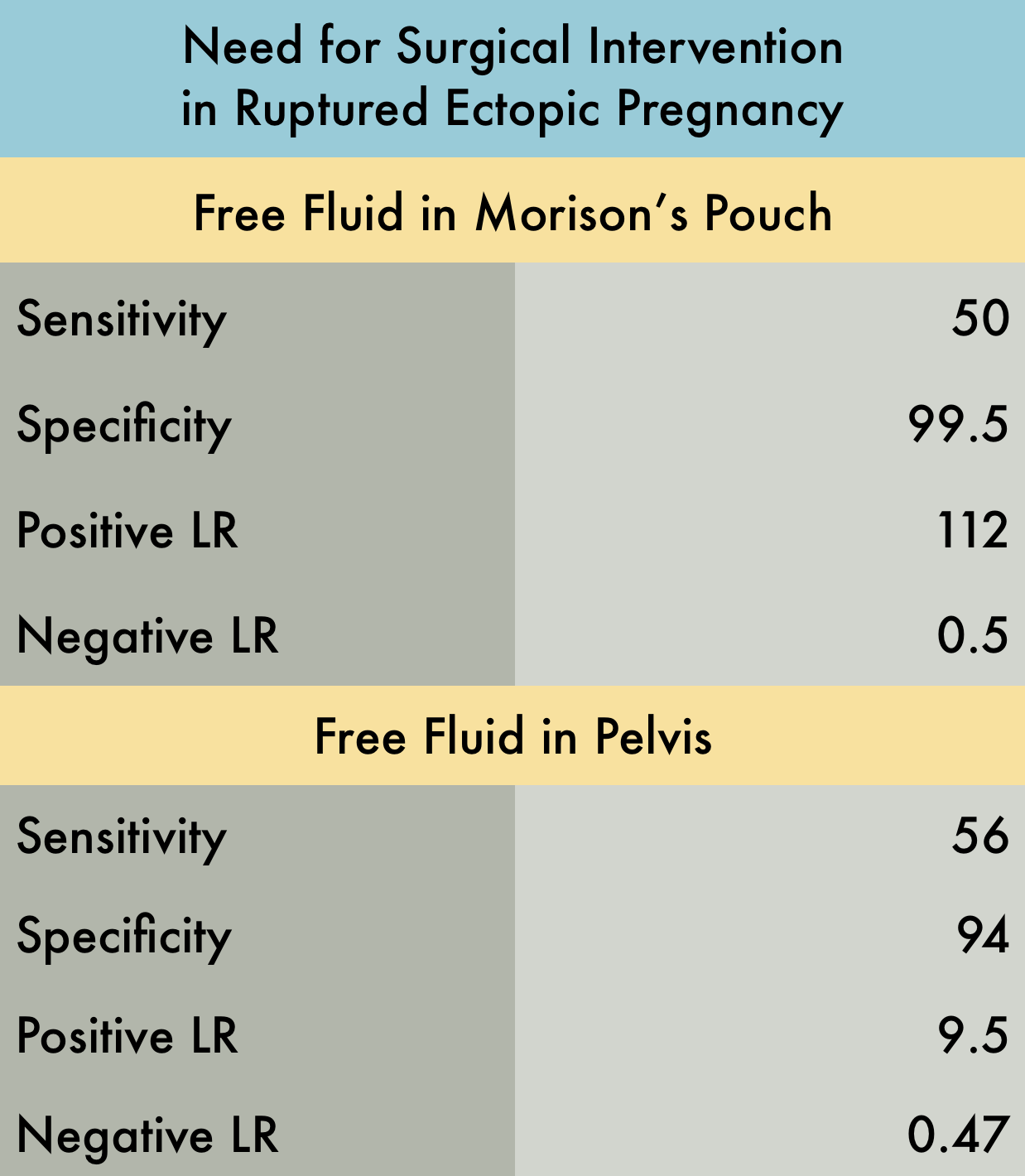
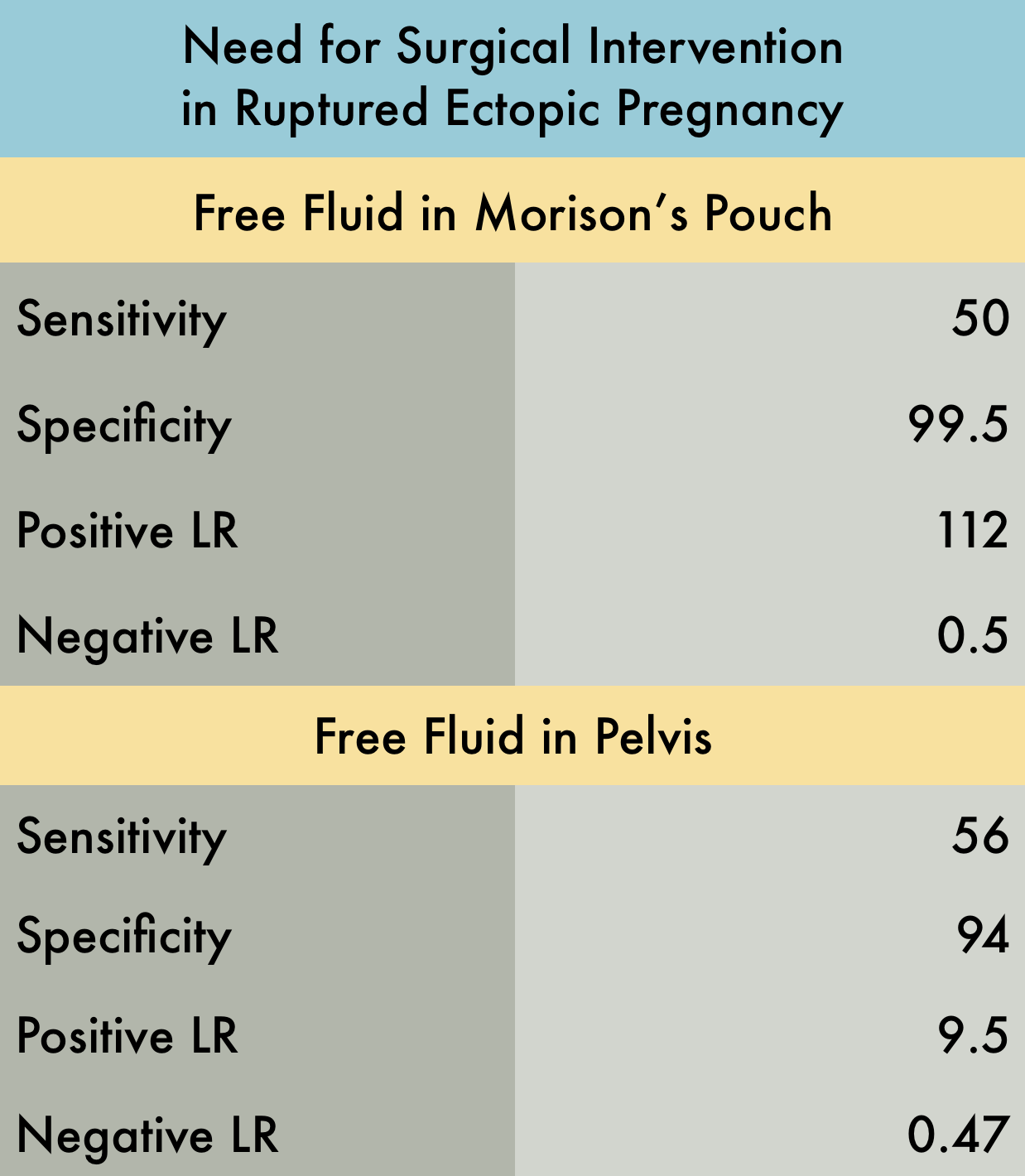
Surgical Intervention in Ruptured Ectopic
This was a prospective observational study (n=242) of patients presenting to the emergency department with suspected ectopic pregnancy, evaluating if free fluid in the peritoneal cavity identified by bedside ultrasound was predictive of the need for operative intervention. The included patients were suspected to have an ectopic pregnancy based on positive pregnancy test results, in their first trimester, with either abdominal pain or vaginal bleeding. All examinations were performed by emergency providers (EPs) using a transabdominal approach, to determine if free fluid was present in the hepatorenal space (Morison’s Pouch) and/or pelvis. Reference standard was chart review by one of four study investigators who were blinded to the EP performed US results. There was one patient who had free fluid in Morison’s Pouch but had a confirmed IUP (suspected to be a ruptured corpus luteum cyst) and no ruptured ectopic pregnancy. This study supports that free fluid present in Morison’s pouch in patients with suspected ectopic pregnancy strongly predicts the need for operative intervention.
PMID: 17554008
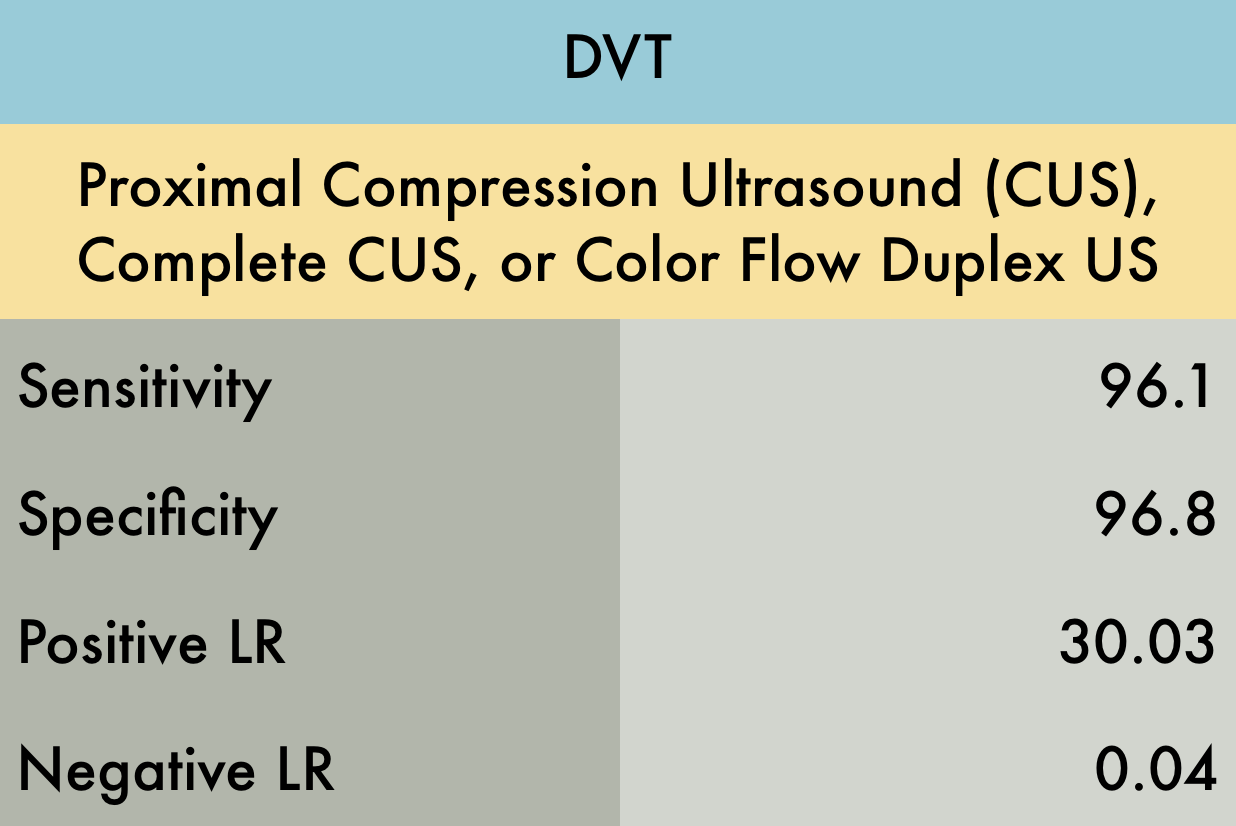
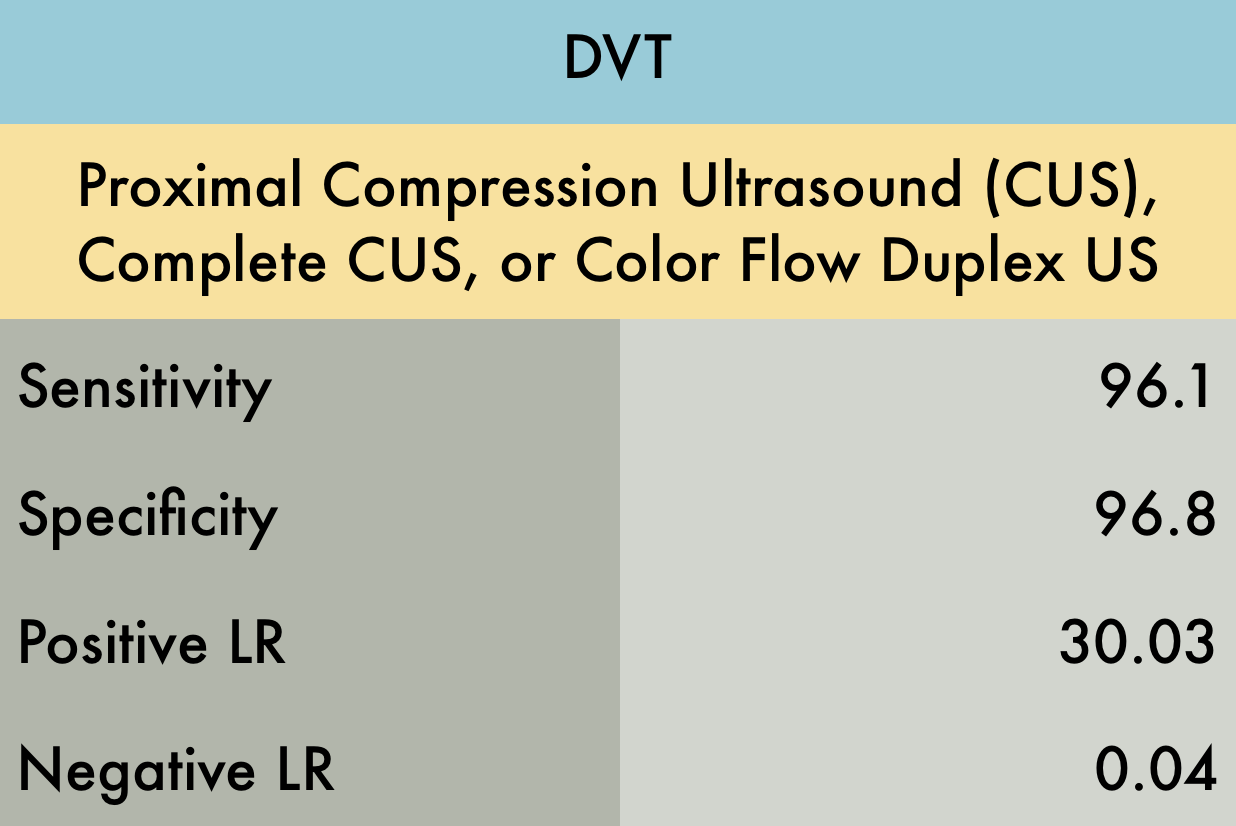
DVT
This was a meta-analysis including 16 studies (n=2379) evaluating the operating characteristics of emergency physician (EP) performed ultrasound for the diagnosis of DVT. The providers used color-flow duplex ultrasound in two studies, proximal venous ultrasound in 13 studies (not looking at the calf), and whole-leg venous ultrasound in one study. Reference standard was radiology department ultrasound, vascular lab, or angiography. Considering only high quality studies which met QUADAS-2 Criteria (11 out of 16 initially selected studies), the sensitivity and specificity improved to 97.6% and 96.8% respectively.
PMID: 23138420
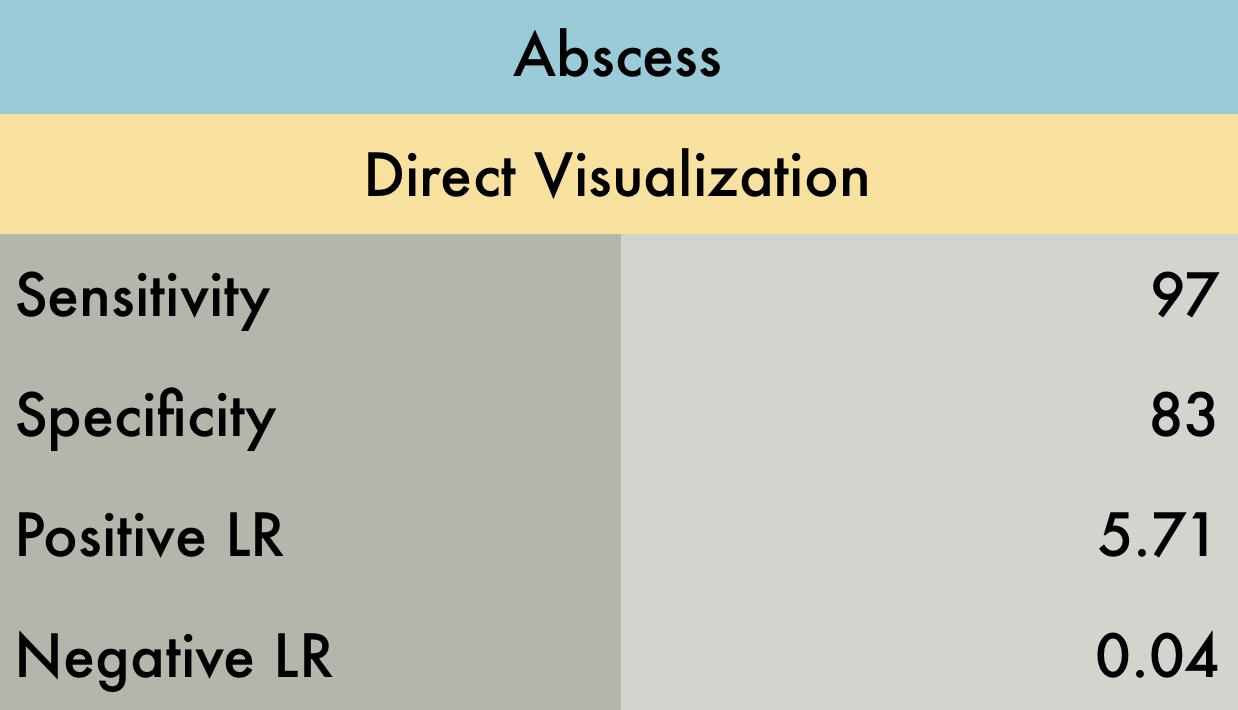
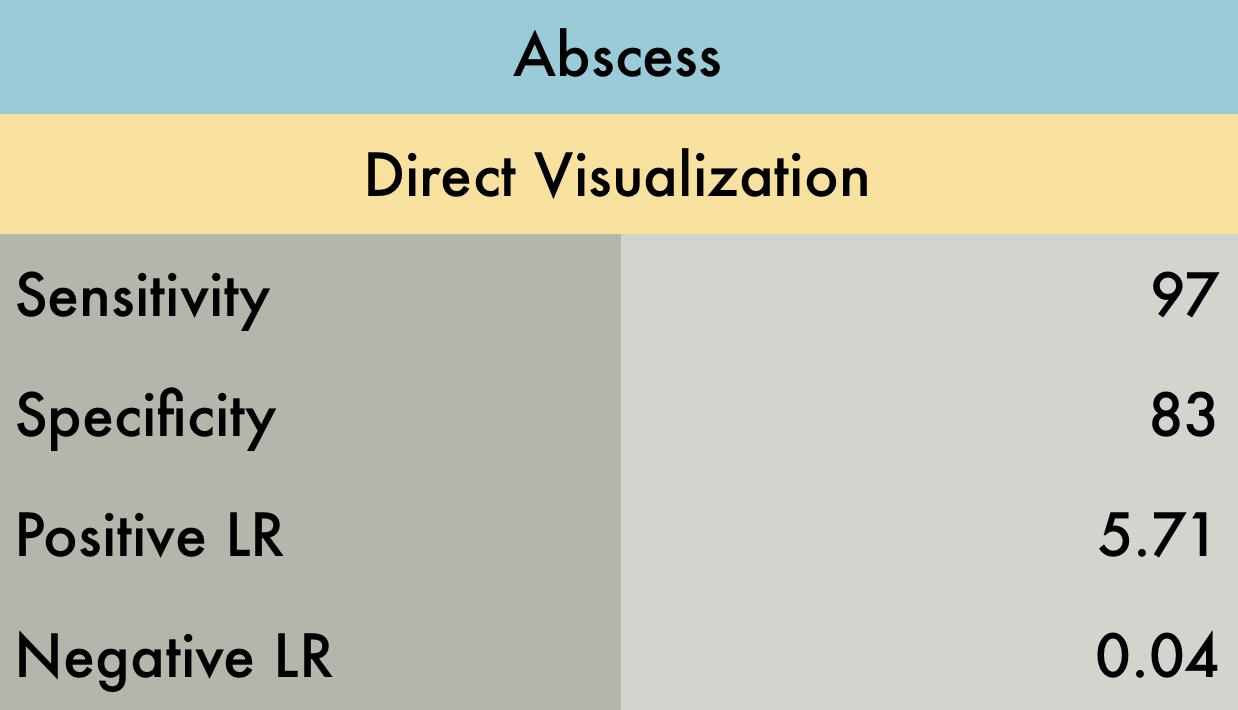
Abscess
This was a systematic review including 6 prospective observational studies (n=800) comparing physical exam and POCUS to diagnose abscess in both children and adults in the emergency department (ED). Inclusion criteria for all but one study was the presence of a skin & soft tissue infection (SSTI) while once study specifically included patients where abscess was suspected with plan to incise and drain. The reference standard for abscess was pus drainage on initial I&D or at follow up. In many studies, facial and genital/rectal area SSTIs were excluded therefore these results should be interpreted with caution in evaluation of SSTIs in these areas.
PMID: 27770490
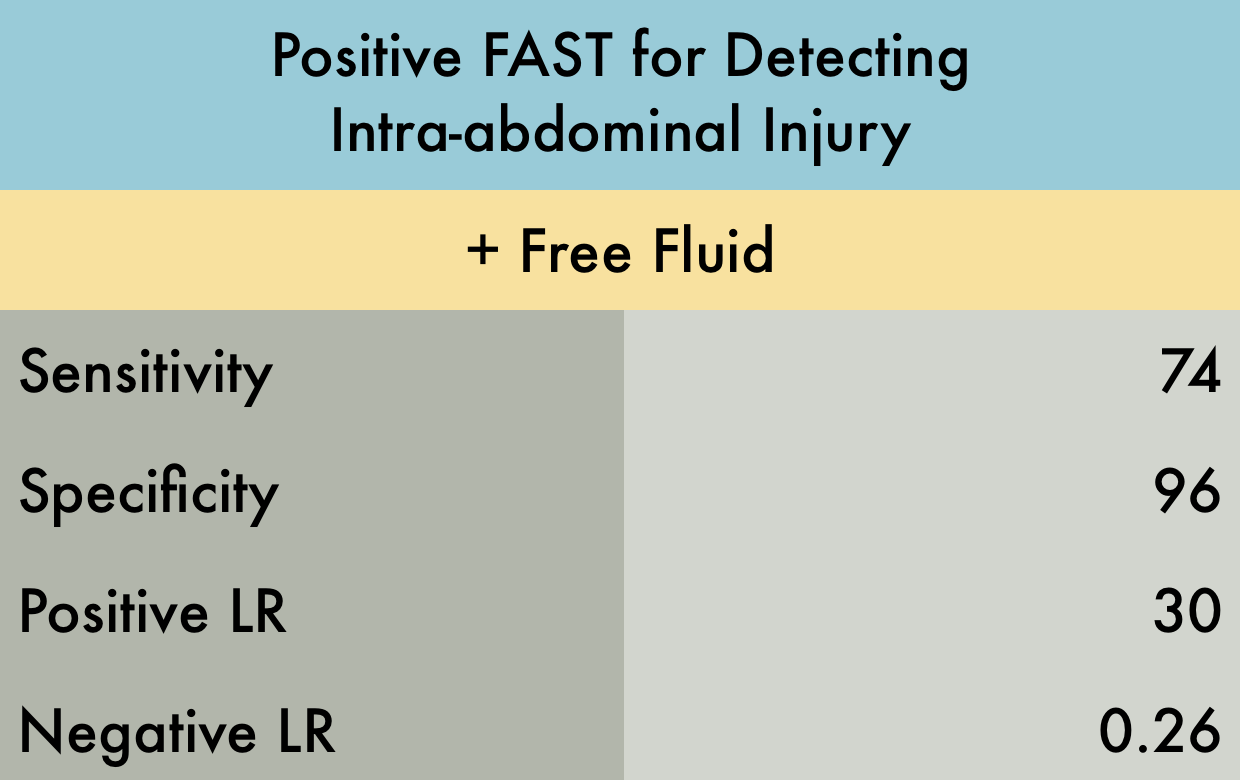
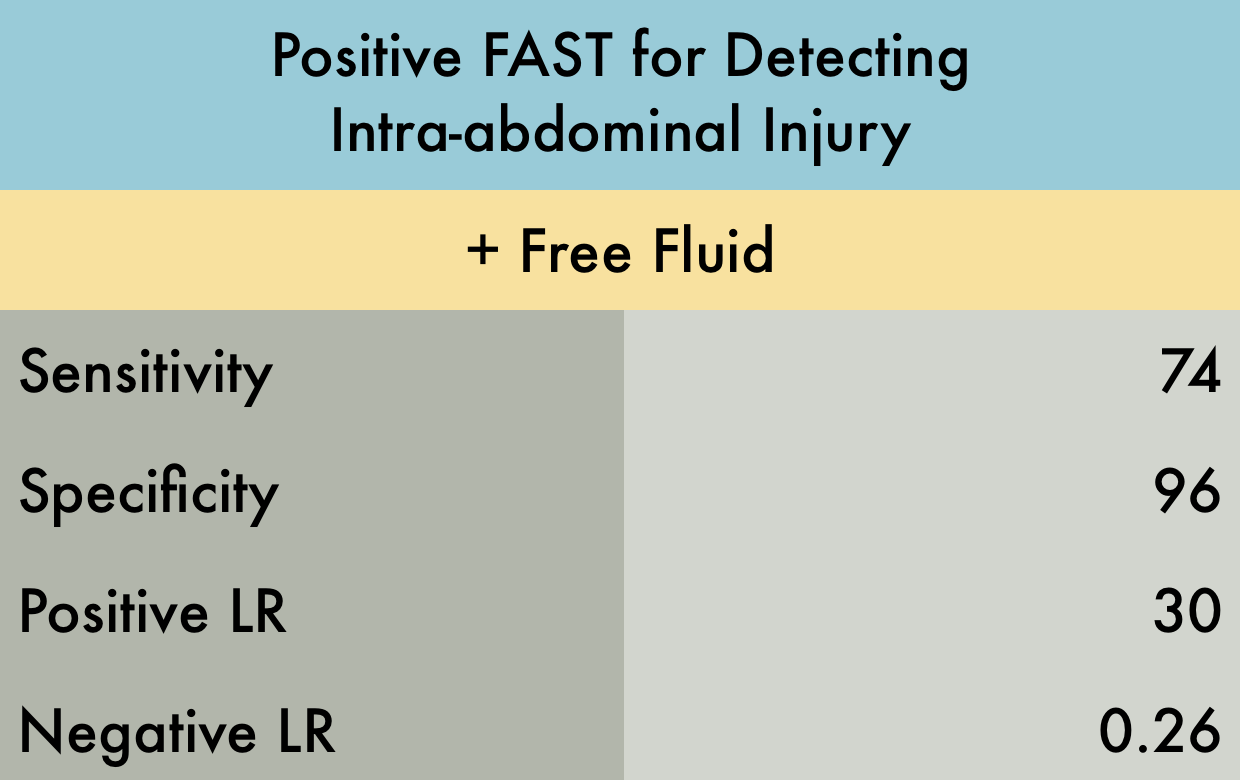
FAST Exam
This was a meta-analysis including 22 studies (n=12089) in adult patients presenting with blunt trauma, evaluating the accuracy of the FAST examination for the detection of intra-abdominal injury. All included studies had at least 1 reference standard including abdominal computed tomography, diagnostic peritoneal lavage, laparotomy, autopsy, and/or clinical course. 5 of the studies excluded patients with hemodynamic instability. When these studies were looked at alone, the positive LR increased to 82.
PMID: 22496266
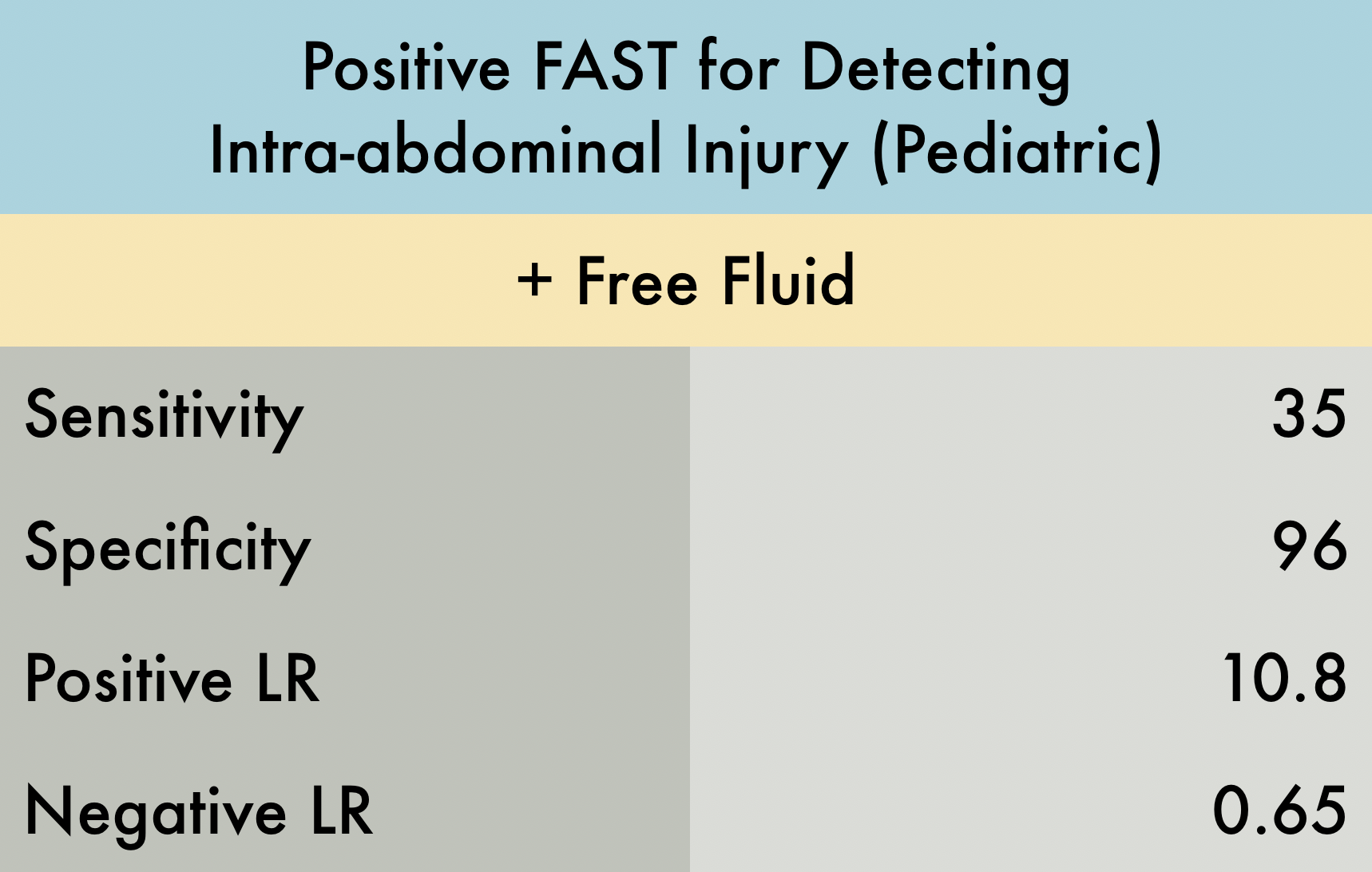
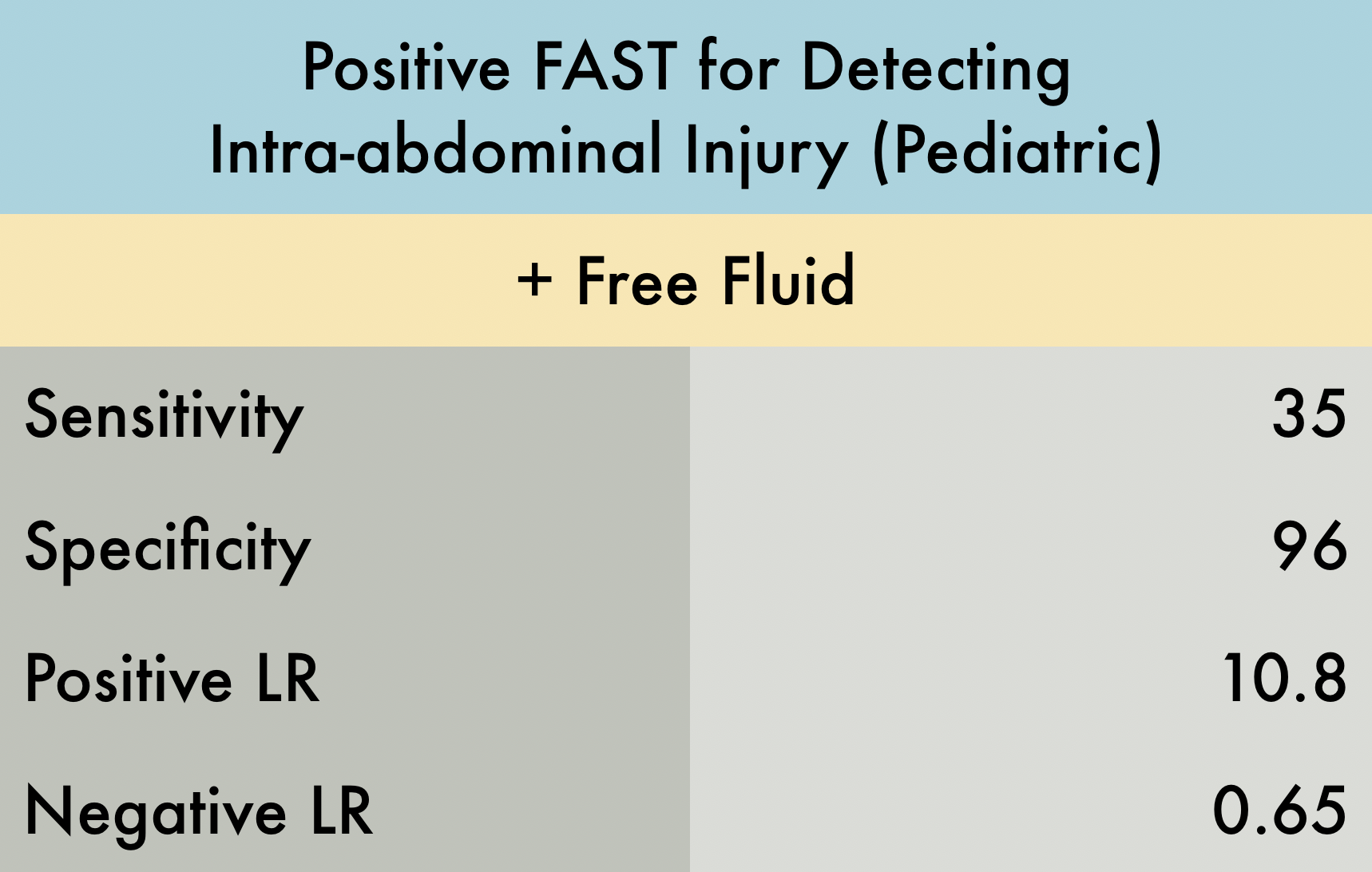
Pediatric FAST Exam
This was a systematic review and meta-analysis including 8 studies (n = 2135) to evaluate the utility of FAST examination in the diagnosis of intra-abdominal injury (IAI) in pediatric blunt abdominal trauma patients. All included studies used 3 different reference standards, which introduced bias by not equally categorize a patient as disease positive or negative. Inclusion criteria for age across these 8 studies ranged from an upper limit of 13 to 18 years old. Index test was presence of any amount of free fluid in hepatorenal, splenorenal, or suprapubic windows during FAST. Reference standards were laparotomy, CT, or observation. Sensitivity was highly variable across 8 studies (20-80%) and found to have a pooled sensitivity of 35%. Specificity remained very high, 96%. Overall, this systemic review found that a negative index test alone cannot rule out the need for further imaging in pediatric intra-abdominal trauma. PMID: 30870341
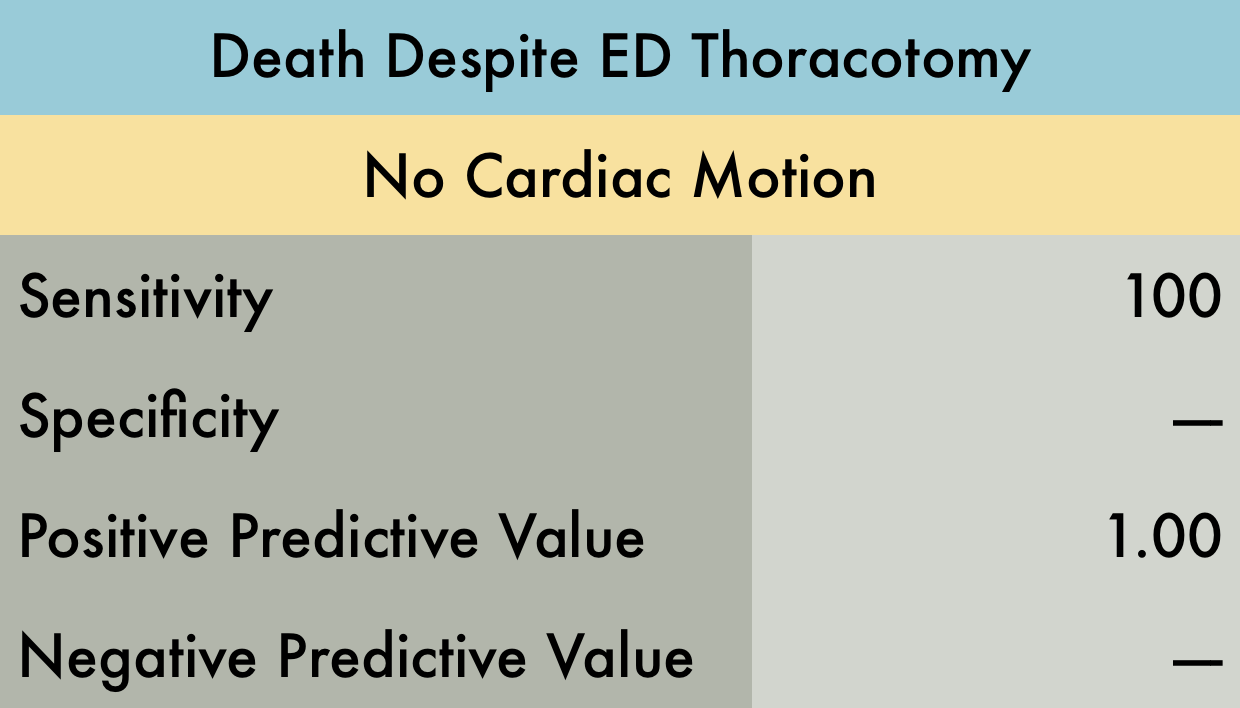
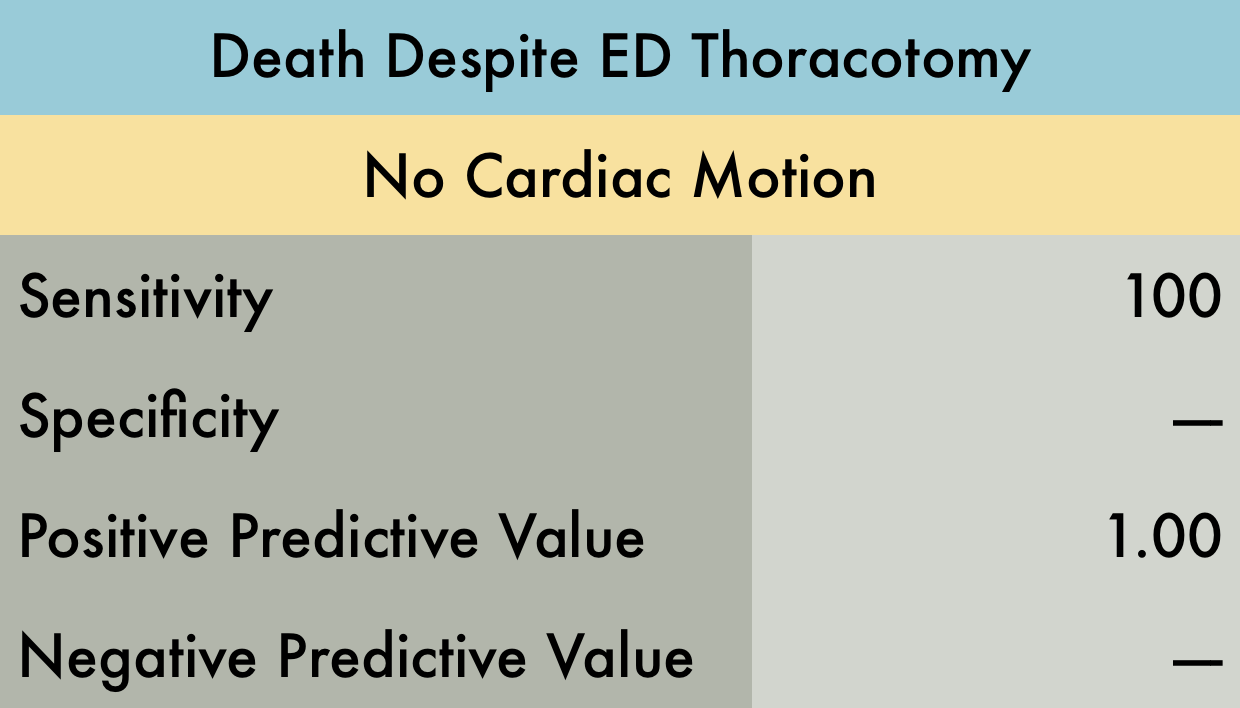
Death Despite ED Thoracotomy
This was a prospective study (n=187) at a Level I trauma center evaluating the utility of resuscitative thoracotomy (RT) in acute trauma patients. A bedside FAST exam was performed before or concurrent with RT. The bedside FAST exam evaluated for cardiac motion and/or pericardial effusion. A sensitivity analysis utilizing the primary outcome measures of survival to discharge or organ donation was performed. Only the outcome of survival to discharge is provided in the accompanying table. Note that Positive Predictive Value was used in provided table as this is easier to interpret with respect to their data. Positive predictive value is the probability that subjects with a positive screening test truly have the disease. With respect to the study data, positive predictive value represents the probability that a patient WILL NOT survive following RT if they have no cardiac activity on bedside echo.
PMID: 26258320
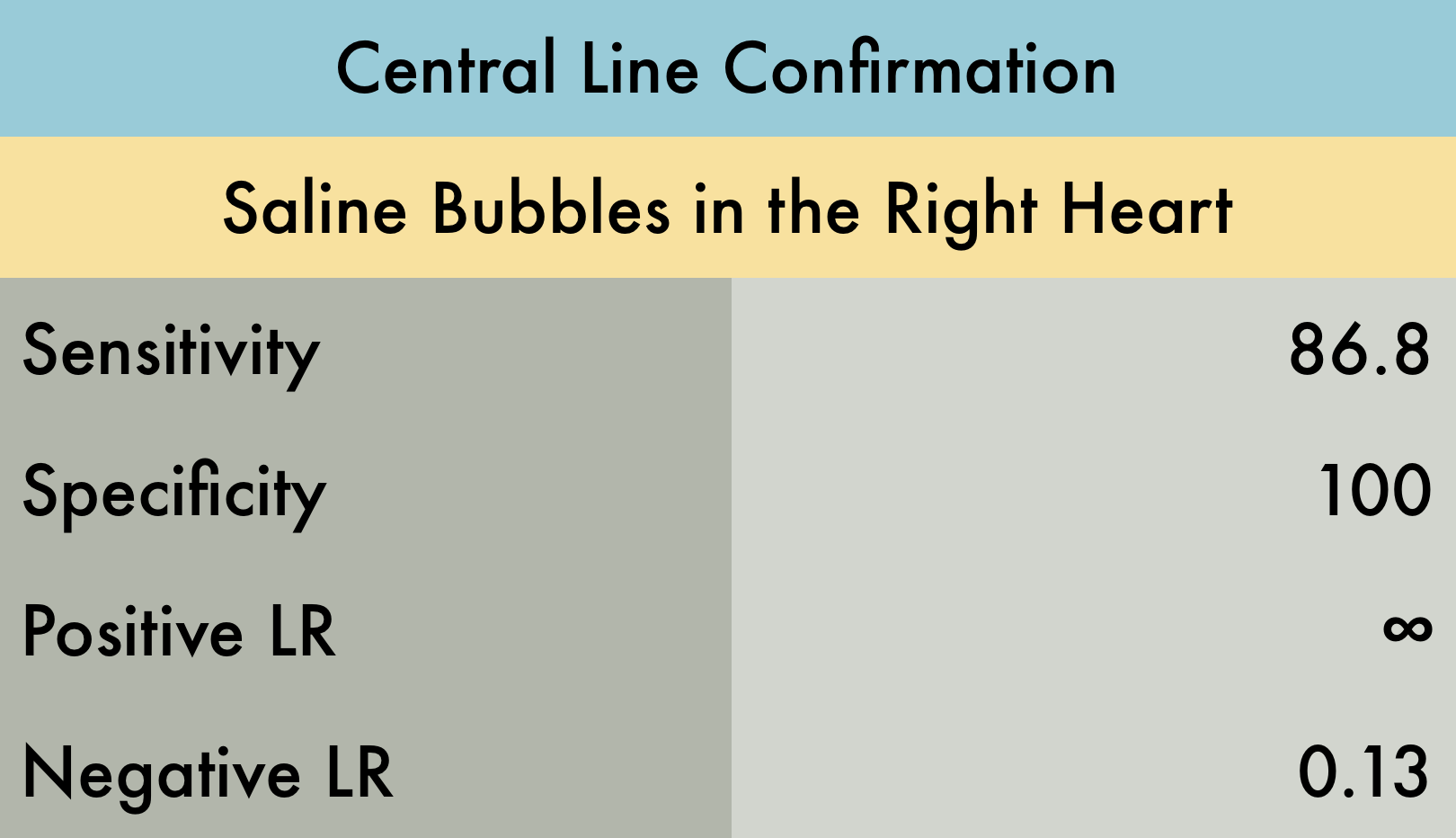
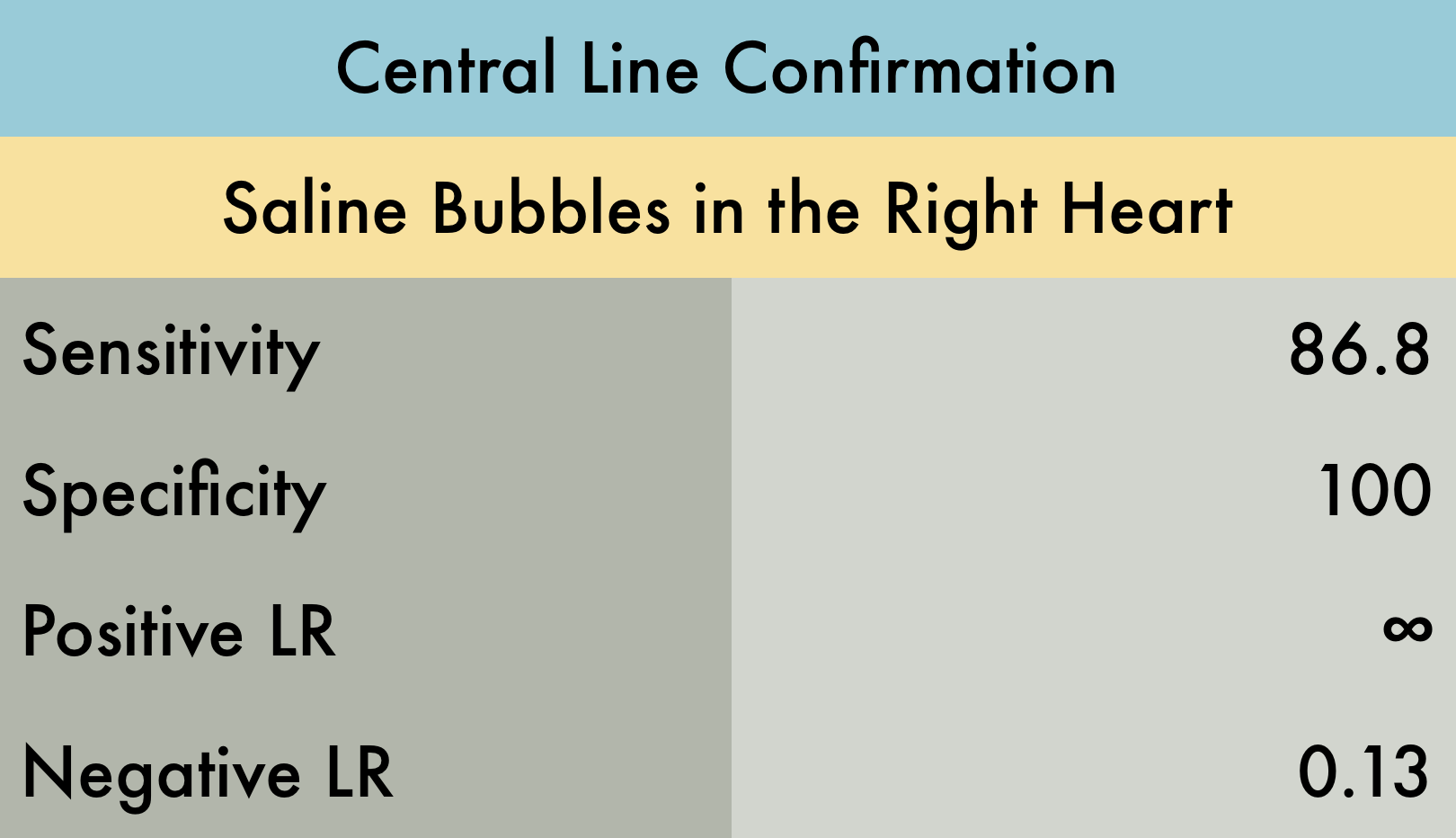
Central Line Confirmation
This was a prospective study (n=78) in critically ill patients in the emergency department (ED) and intensive care unit (ICU) at a single academic center, evaluating the use of POCUS to identify correct placement of supra-diaphragmatic central venous catheter (CVC) placement. All CVC placements and POCUS exams were performed by resident trainees. Correct positioning of the CVC was considered if turbulent flow was visualized in the right atrium on sub-xiphoid, parasternal, or apical cardiac ultrasound after injecting 5 cc of sterile, non-agitated, normal saline through the CVC. Reference standard was confirmatory chest radiography.
PMID: 28123616
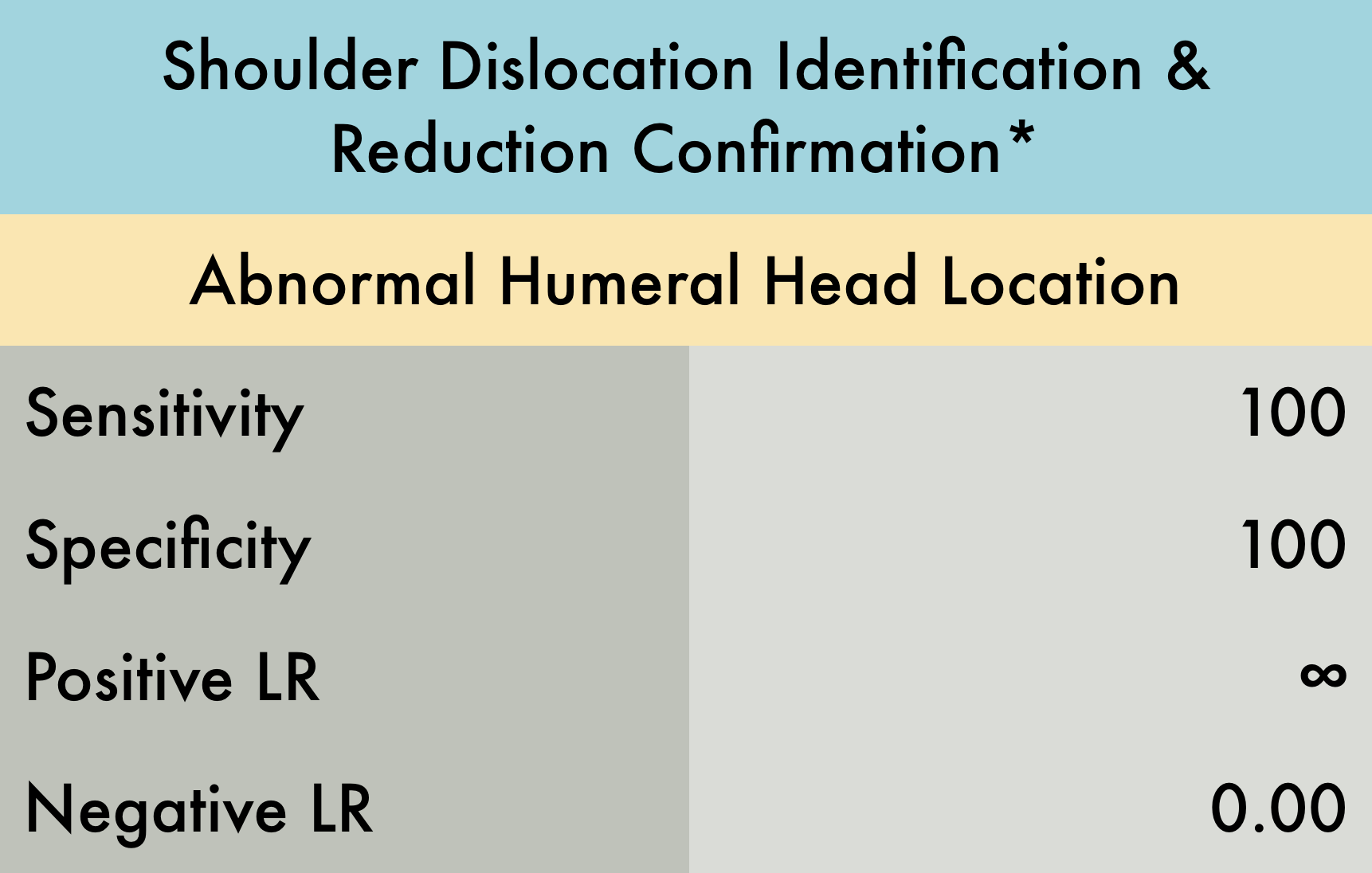
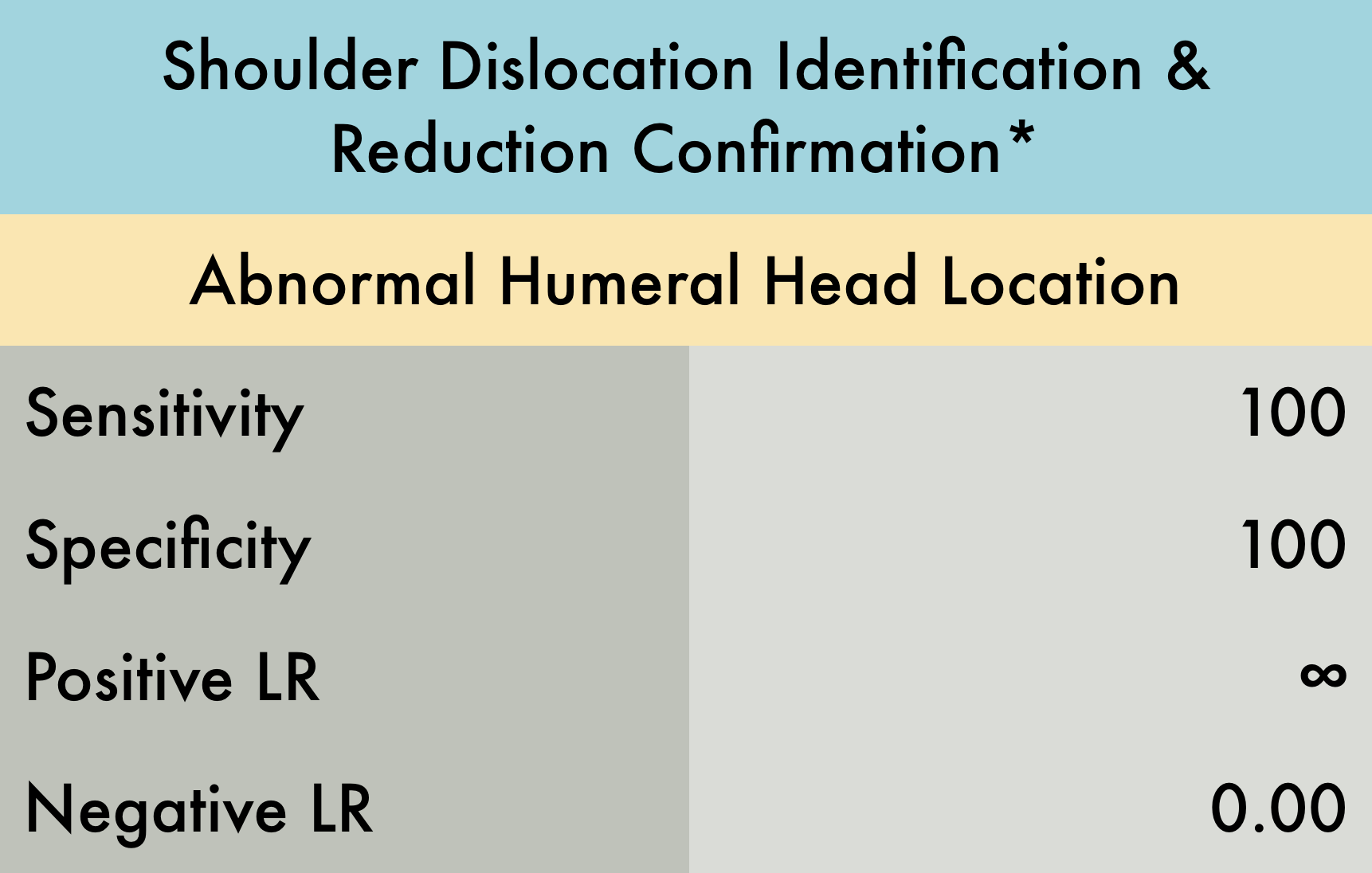
Shoulder Dislocation
This was a prospective observational study (n= 73) evaluating the diagnostic accuracy of ultrasound for both identification of shoulder dislocation and confirmation of successful reduction. Patients with suspected shoulder dislocation were enrolled, with 69/73 having dislocation confirmed by shoulder radiographs. Patients with multi trauma or decreased level of consciousness were excluded. Both the anterior and lateral approach were used to evaluate for dislocation. Examinations were performed by either an experienced ultrasound trained emergency physician or a senior emergency medicine resident. An ultrasound exam was performed prior to initial shoulder radiographs and after reduction attempt. Ultrasound was found to be 100% accurate with respect to both shoulder dislocation identification and reduction confirmation. *This is a limited study as the sample size is relatively small and this ultrasound examination is dependent on operator experience therefore these results should be interpreted with caution.
PMID: 23489654
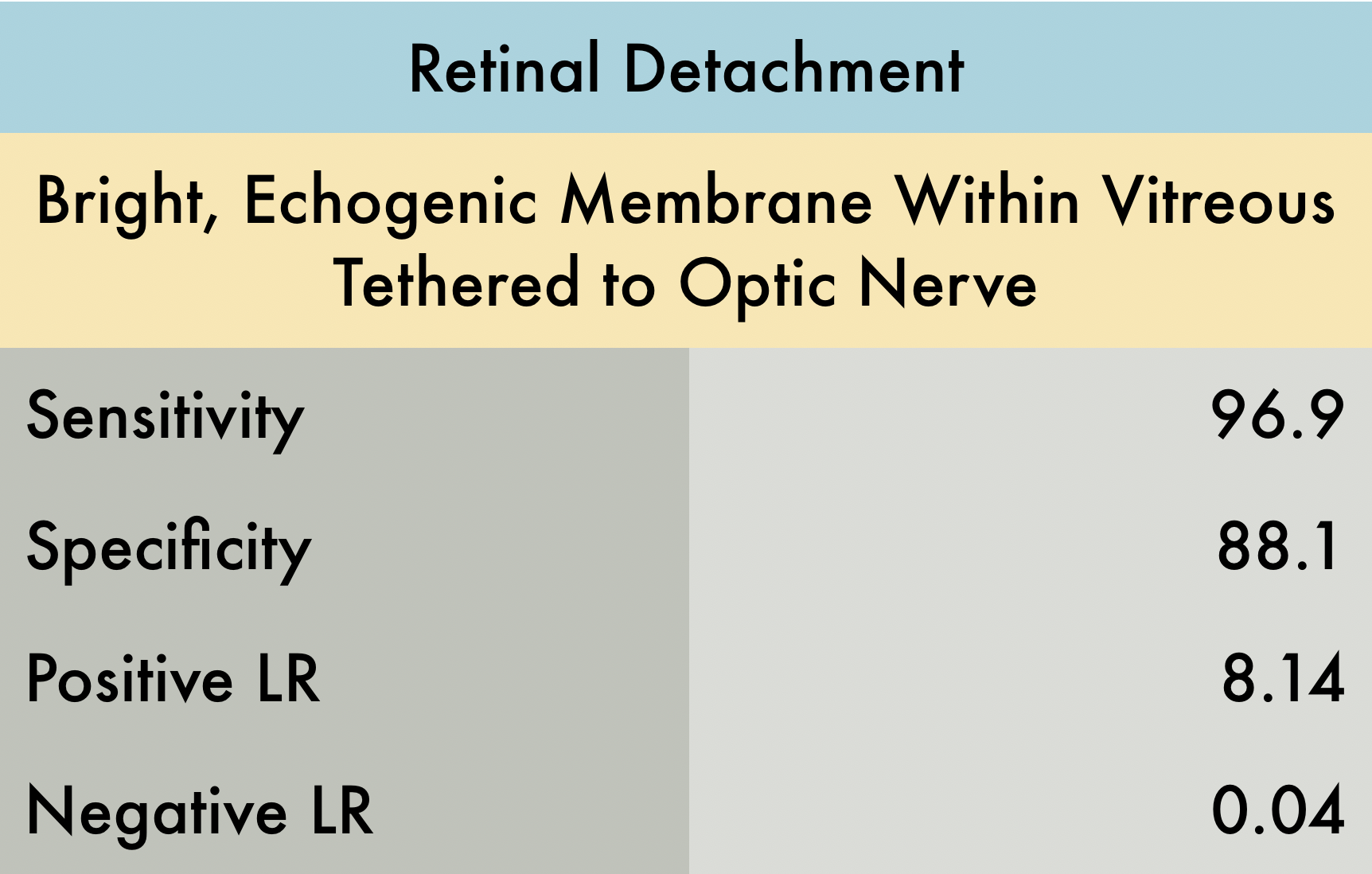
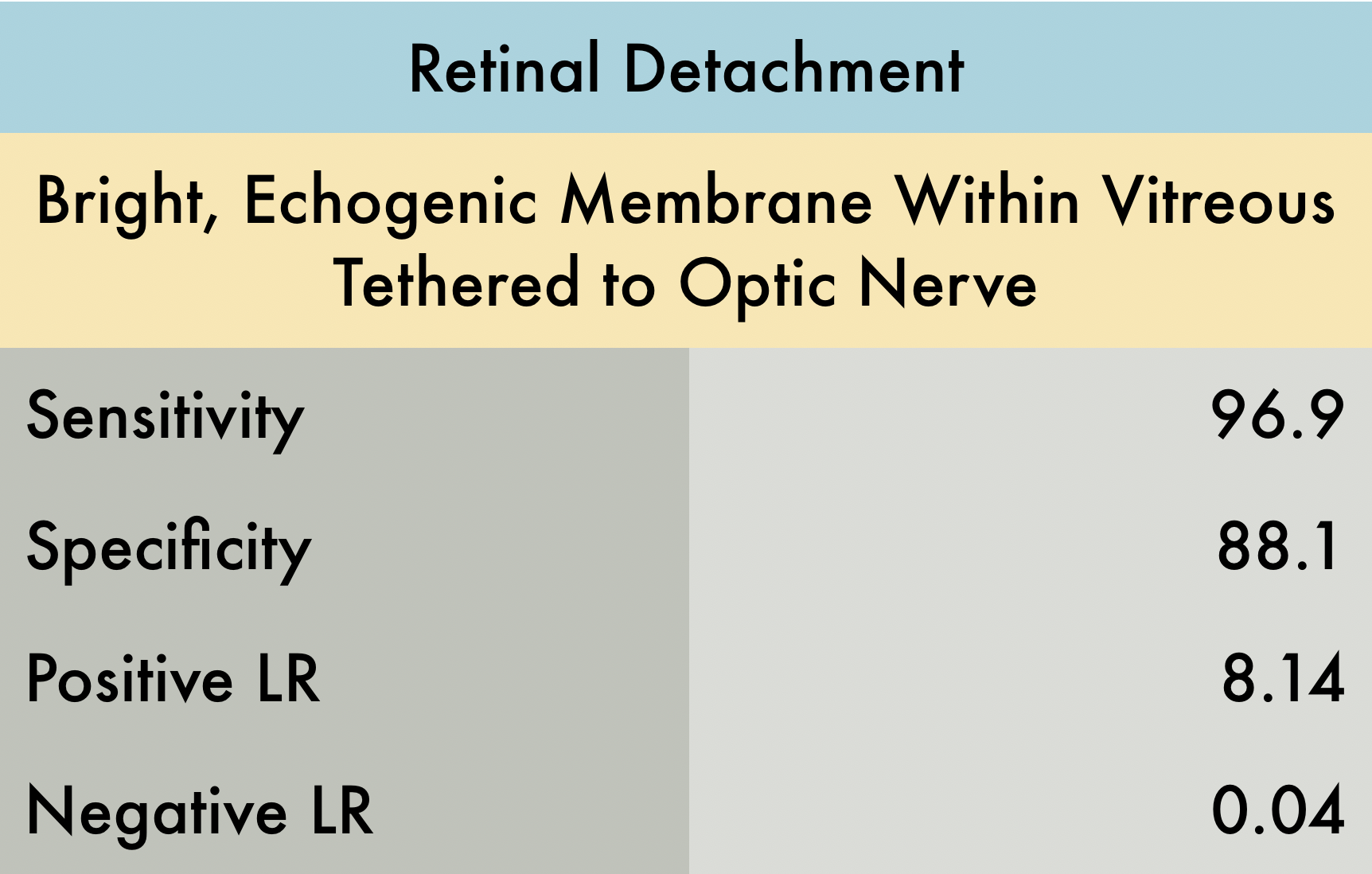
Retinal Detachment
This was a prospective, multi-center study conducted at 2 academic emergency departments (ED) and 2 county hospital EDs (n = 225) to evaluate the accuracy of POCUS for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD). Each hospital recruited patients presenting to the ED with symptoms of blurry vision, flashers/floaters, and vision loss, whom required emergent ophthalmologic consultation; patients with ocular trauma or suspected globe rupture were excluded. Reference standard was attending ophthalmologists’ final diagnosis masked to POCUS results. Exams were performed by seventy-five unique providers including seventy emergency physicians of varying training level and 5 physician assistants. Study findings demonstrate that the utility of ED POCUS in the diagnosis for RD and VH were quite sensitivity and specific. The utility of POCUS in the diagnosis of VD was less sensitive (42.5%) but remained specific (96%). Overall, ocular POCUS by ED providers is a very good test to both rule-in and rule-out the emergent diagnosis of RD. The use of ocular POCUS is not as good of a test to rule-in or rule-out less emergent diagnoses of VD and VH but provides useful adjunct information to support evidence for those diagnoses. PMID: 30977855 - Reviewed by Dr. Jaclyn Walker
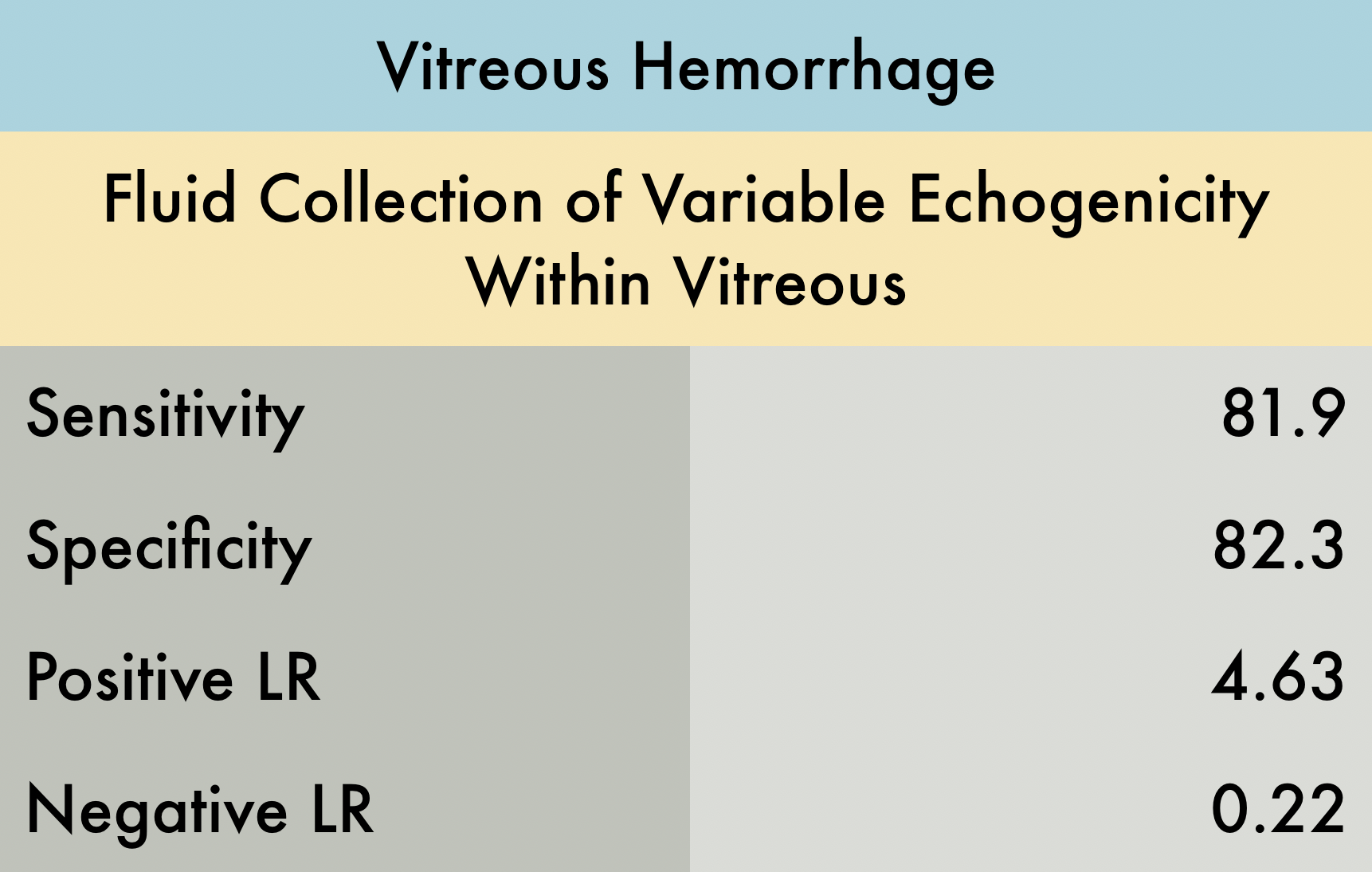
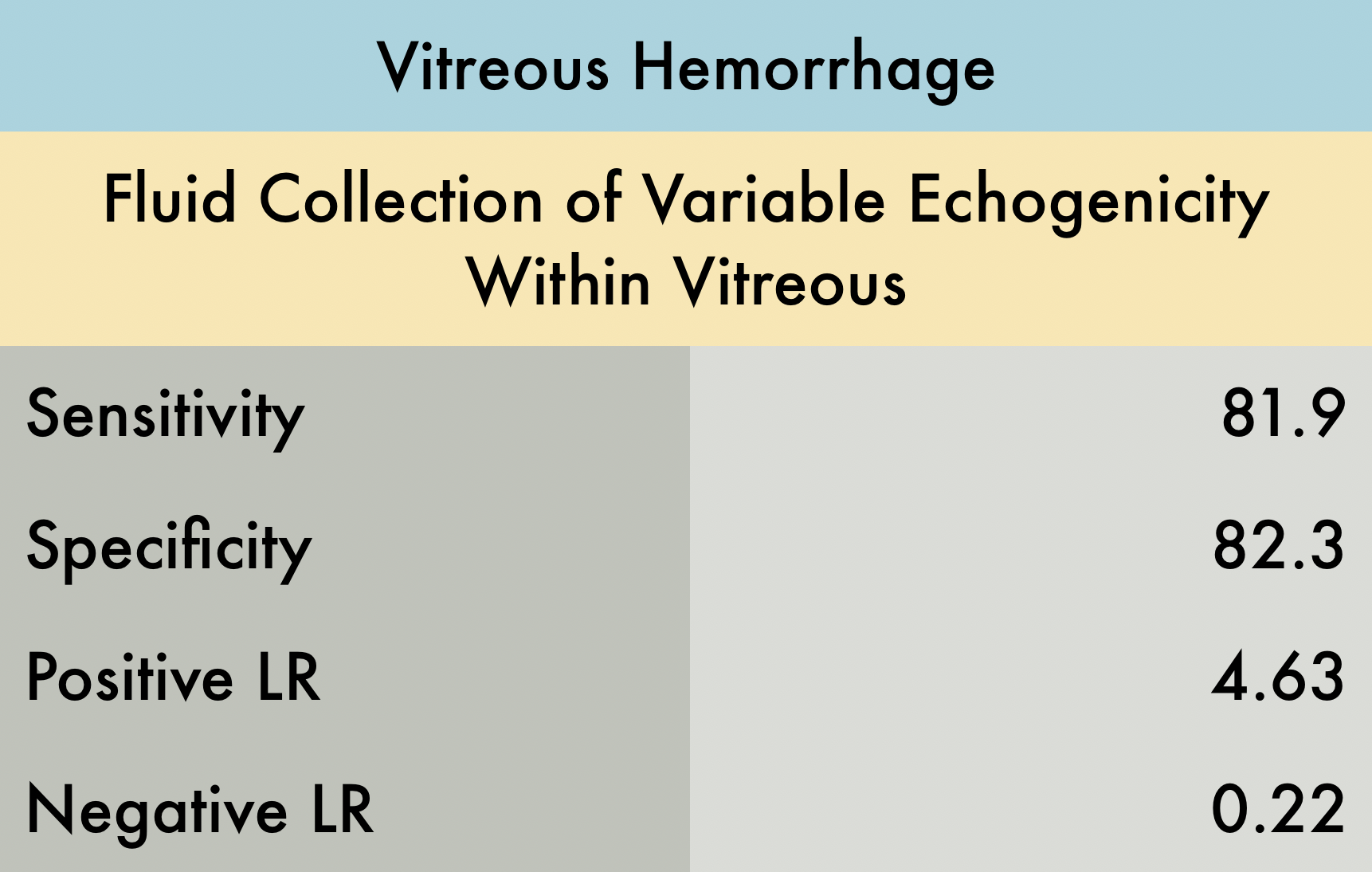
Vitreous Hemorrhage
This was a prospective, multi-center study conducted at 2 academic emergency departments (ED) and 2 county hospital EDs (n = 225) to evaluate the accuracy of POCUS for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD). Each hospital recruited patients presenting to the ED with symptoms of blurry vision, flashers/floaters, and vision loss, whom required emergent ophthalmologic consultation; patients with ocular trauma or suspected globe rupture were excluded. Reference standard was attending ophthalmologists’ final diagnosis masked to POCUS results. Exams were performed by seventy-five unique providers including seventy emergency physicians of varying training level and 5 physician assistants. Study findings demonstrate that the utility of ED POCUS in the diagnosis for RD and VH were quite sensitivity and specific. The utility of POCUS in the diagnosis of VD was less sensitive (42.5%) but remained specific (96%). Overall, ocular POCUS by ED providers is a very good test to both rule-in and rule-out the emergent diagnosis of RD. The use of ocular POCUS is not as good of a test to rule-in or rule-out less emergent diagnoses of VD and VH but provides useful adjunct information to support evidence for those diagnoses. PMID: 30977855 - Reviewed by Dr. Jaclyn Walker
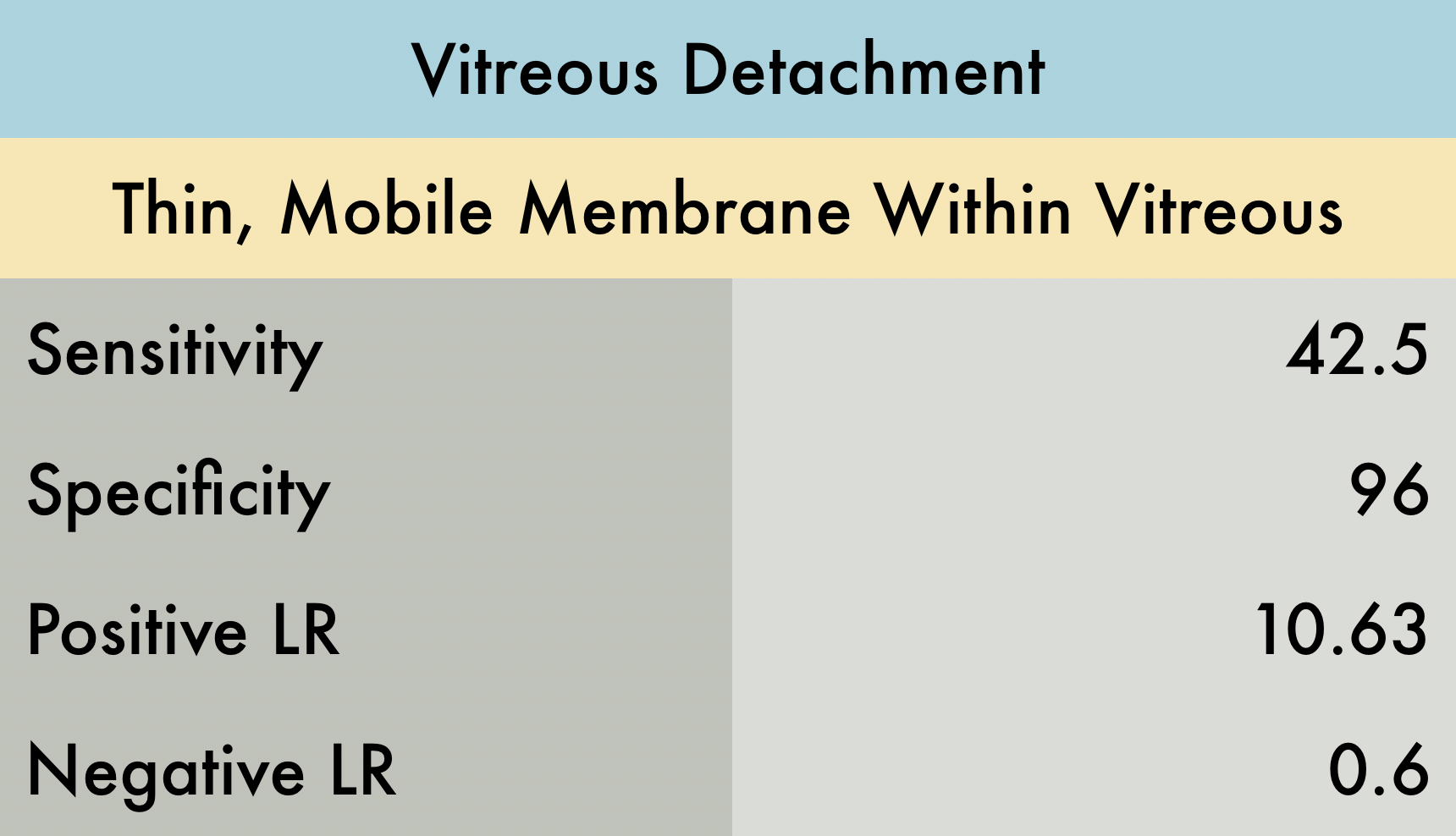
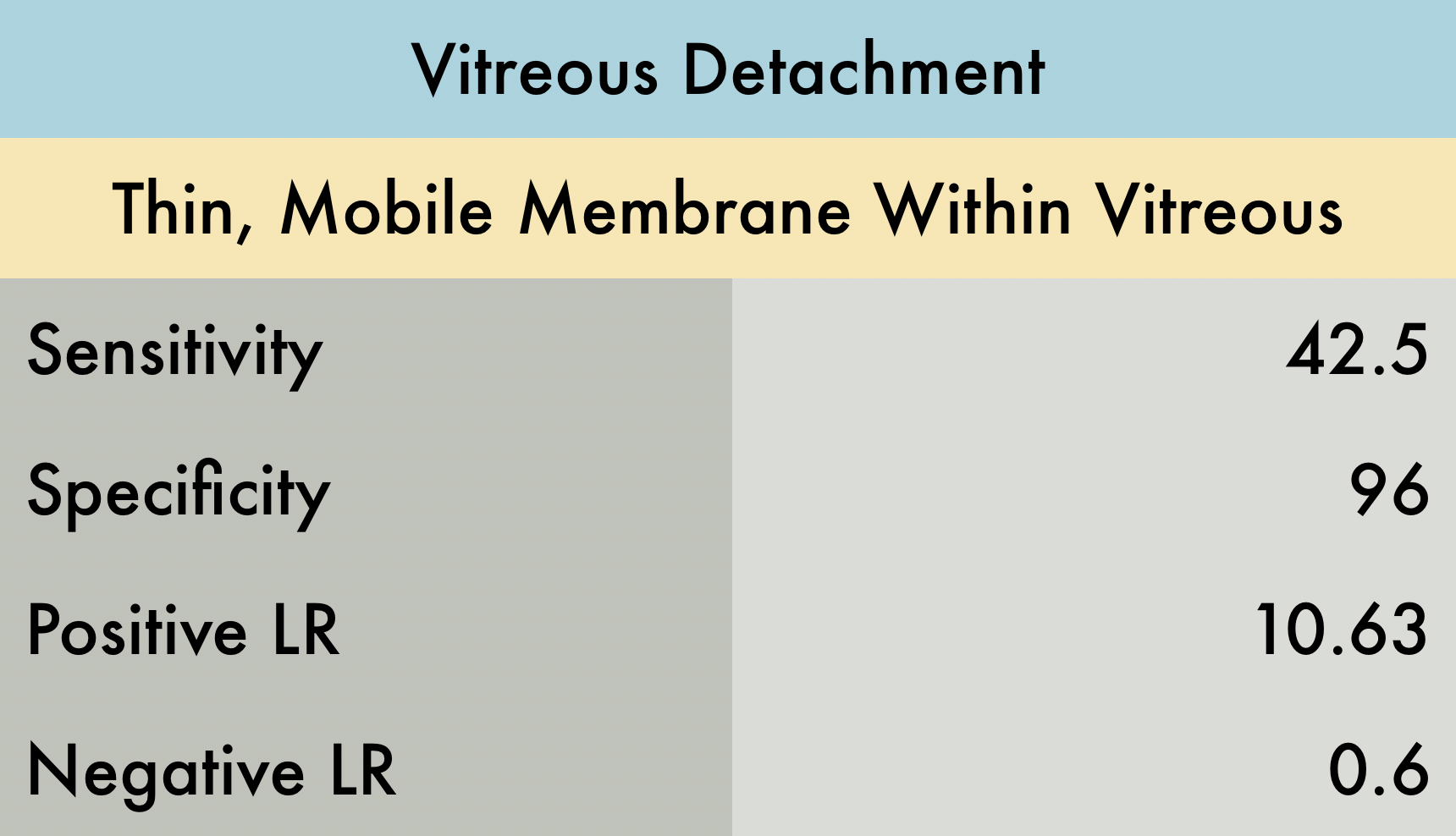
Vitreous Detachment
This was a prospective, multi-center study conducted at 2 academic emergency departments (ED) and 2 county hospital EDs (n = 225) to evaluate the accuracy of POCUS for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD). Each hospital recruited patients presenting to the ED with symptoms of blurry vision, flashers/floaters, and vision loss, whom required emergent ophthalmologic consultation; patients with ocular trauma or suspected globe rupture were excluded. Reference standard was attending ophthalmologists’ final diagnosis masked to POCUS results. Exams were performed by seventy-five unique providers including seventy emergency physicians of varying training level and 5 physician assistants. Study findings demonstrate that the utility of ED POCUS in the diagnosis for RD and VH were quite sensitivity and specific. The utility of POCUS in the diagnosis of VD was less sensitive (42.5%) but remained specific (96%). Overall, ocular POCUS by ED providers is a very good test to both rule-in and rule-out the emergent diagnosis of RD. The use of ocular POCUS is not as good of a test to rule-in or rule-out less emergent diagnoses of VD and VH but provides useful adjunct information to support evidence for those diagnoses. PMID: 30977855
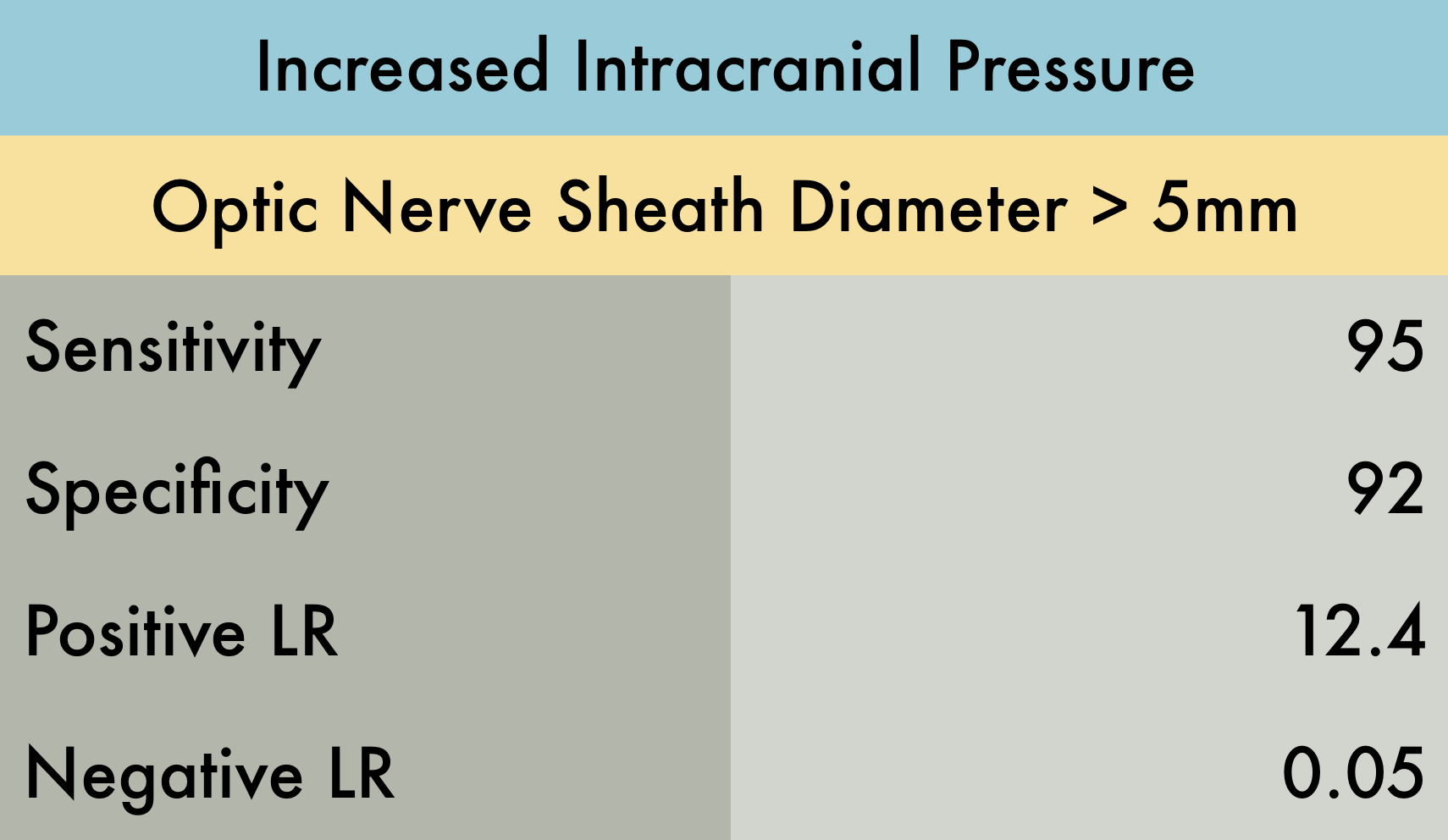
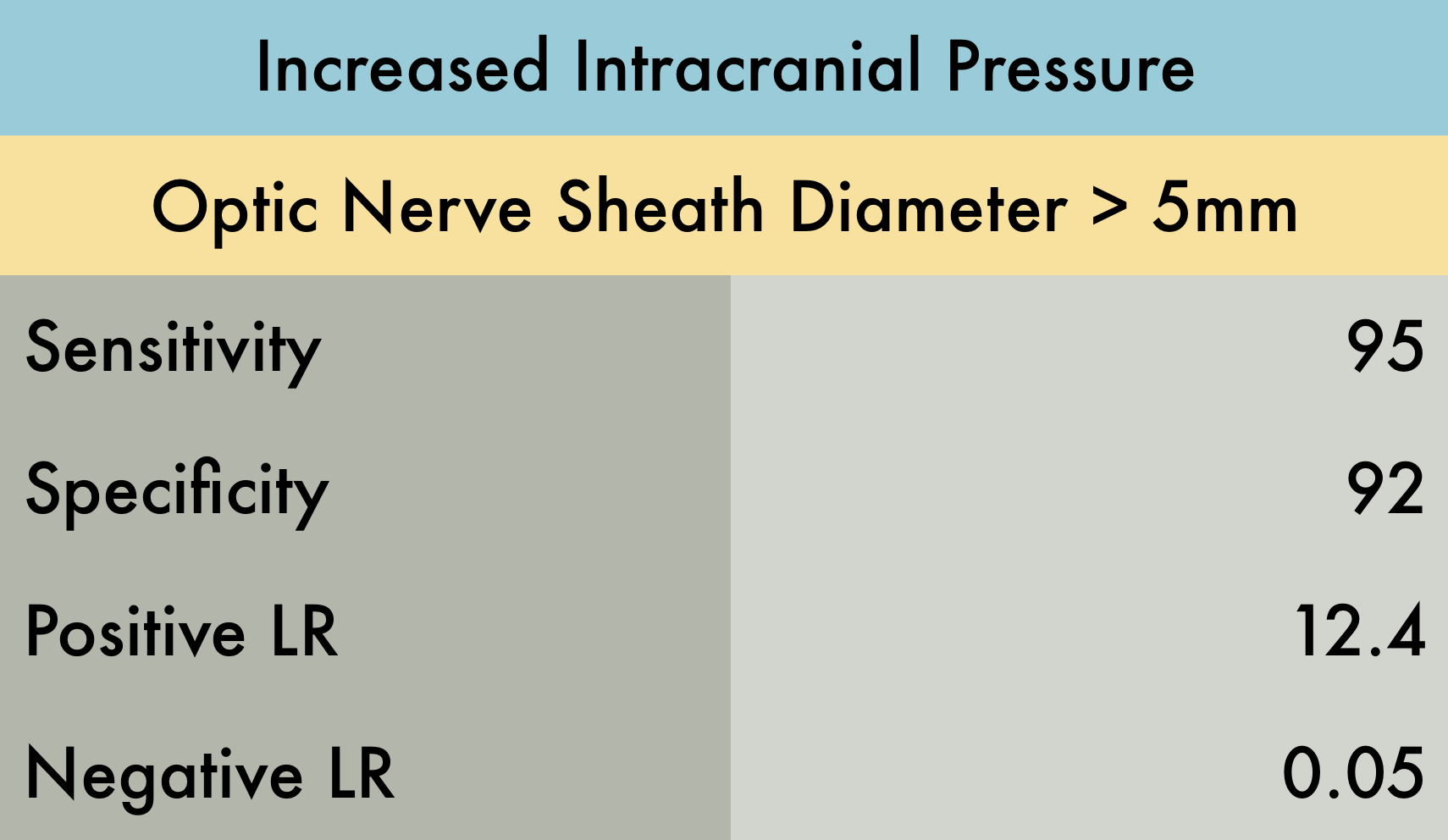
Increased Intracranial Pressure
This was a systematic review, which including 12 studies (n = 478) using ultrasound measurement of optic nerve diameter (cut point of 5 mm for adult studies, 4.5 mm for age 1–17 years, and 4 mm for age <1 year) to evaluate for increased intracranial pressure (ICP). There was moderate to high heterogeneity among these studies given multiple patient populations. This resulted in wide confidence intervals: sensitivity of 95.6% (95% CI, 87.7%–98.5%), specificity of 92.3% (95% CI, 77.9%–98.4%), positive likelihood ratio of 12.5 (95% CI, 4.2–37.5), and a negative likelihood ratio of 0.05 (95% CI 0.016–0.14). It is also important to mention that the gold standard in this review was CT, which is not as accurate as invasive ICP monitoring. Overall their conclusions were that ocular sonography had a very low LR- (0.05) making it a good test for ruling out raised ICP in a low-risk group, and a high LR+ (12.4) making it a good test for ruling in raised ICP in a high-risk group.
PMID: 26112632
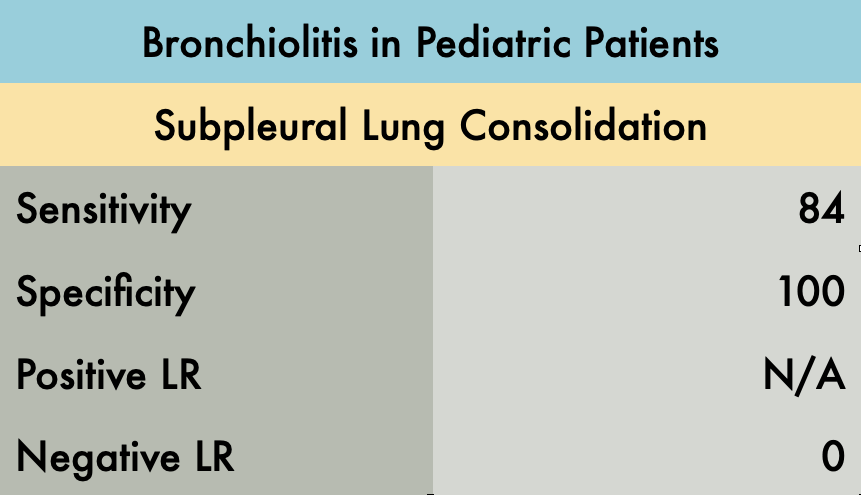
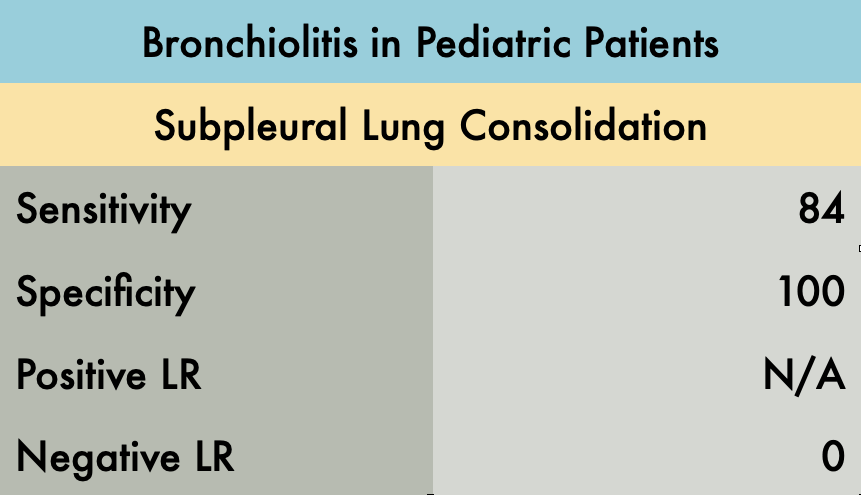
Bronchiolitis in Pediatric Patients
This was a prospective observational study comparing the operating characteristics of emergency department (ED) performed LUS versus CXR for diagnosis of children with bronchiolitis. A total of 52 patients were enrolled in the study. All LUS were performed by one blinded experienced sonographer. Abnormal LUS findings in the study included: subpleural consolidations, b-lines (confluent b-lines or areas of multiple b-lines), and pleural abnormalities. In 44/52 infants with bronchiolitis, subpleural consolidations were present, compared to 0/52 infants without bronchiolitis. Notably, the sensitivity increased from 84% to 90% when all LUS abnormalities are considered (b-lines and pleural irregularities in addition to subpleural consolidation). The presence of multiple areas of lung consolidation and confluent b-lines (white lung) were most predictive of the bronchiolitis severity. CXR was considered positive in 38/52 patients when lung consolidation, peribronchial thickening, or hyperexpansion was identified. Nine patients with a negative CXR but abnormal LUS findings had a clinical course that was consistent with bronchiolitis.
An advantage of LUS in this study was decreased time to diagnosis. LUS was interpreted during the study, while CXR took an average of 4 hours and 45 minutes to interpret after imaging was obtained. Limitations of this study include the small sample size and a single operator for all ultrasounds performed. Bronchiolitis is typically a clinical diagnosis and as such was defined by history and clinical examination in this study. The current study compared LUS to CXR, but there is no gold standard for diagnosing bronchiolitis.. These limitations make the specificity of 100% questionable and indicate the need for larger studies.
PMID: 21468639
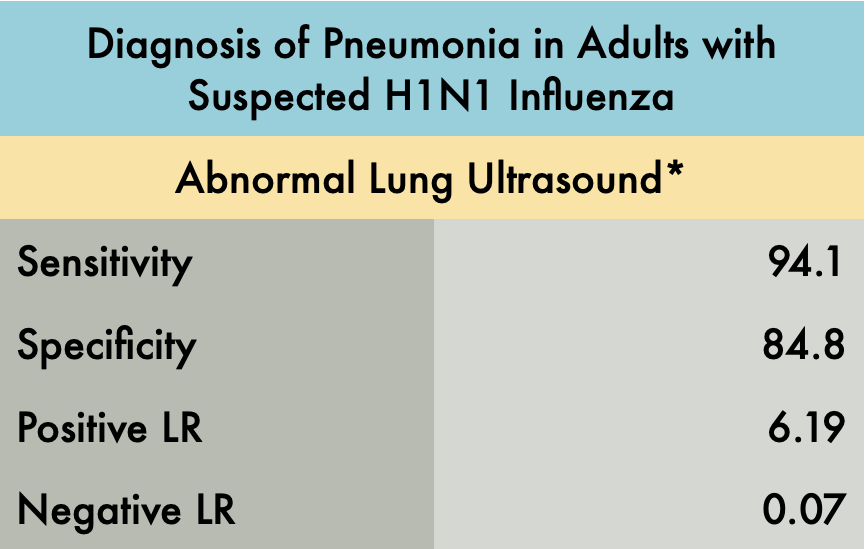
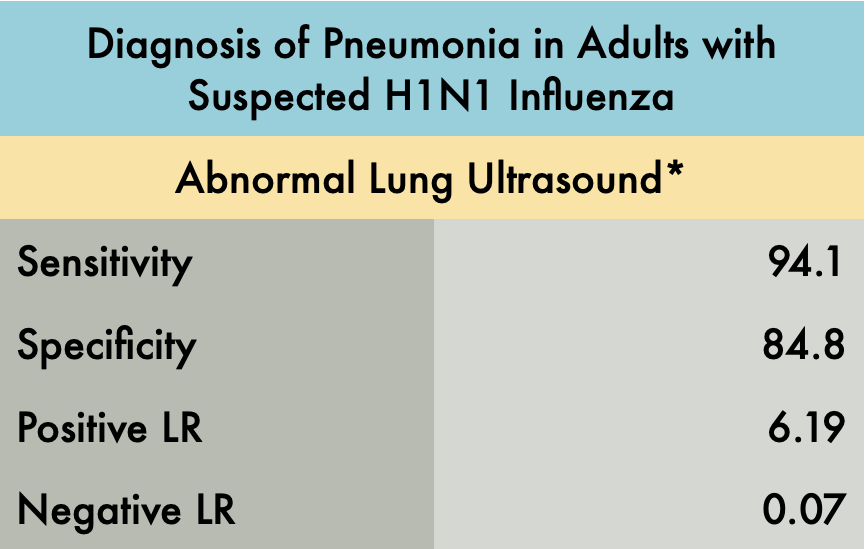
Diagnosis of Pneumonia in Adults with Suspected H1N1 Influenza
This was a prospective observational study comparing the operating characteristics of emergency department (ED) performed LUS versus CXR for the diagnosis of pneumonia in patients with suspected H1N1 influenza. The operating characteristics described in the table include patients with any pneumonia: primary bacterial pneumonia, viral (H1N1) pneumonia, or a secondary bacterial pneumonia in H1N1 infected patients. Patients were included in the experimental arm if they had signs or symptoms of influenza-like illness (ILI) with suspicion of lung involvement (pneumonia), either bacterial or viral. A total of 87 patients were enrolled in the study, 41 with ILI with suspected pneumonia and 46 with ILI without suspected pneumonia (control group).
The gold standard final diagnosis of pneumonia was based on the chart review of the hospital course including the history, physical exam, lab results, and radiographic findings. The reviewers were blinded to the LUS results. Three outcomes were reported: viral pneumonia with laboratory confirmation of the H1N1, primary bacterial pneumonia, or secondary bacterial pneumonia with confirmed H1N1.
The LUS studies were performed by three different emergency physicians with greater than 10 years of ultrasound experience. This study evaluated each hemithorax in five areas: two anterior, two lateral, and one posterior. The presence of any of the following signs on LUS indicated an abnormal exam*:
>3 B-lines per intercostal space
Thickness of pleural line > 2mm or coarse appearance
Consolidation or hepatization
Pleural effusion
Lung ultrasound showed a sensitivity of 94.1% and specificity of 84.8%. An abnormal ultrasound was present in 32 of 34 patients with the ultimate diagnosis of pneumonia (including viral and bacterial). In patients with initially negative CXRs, 15/16 demonstrated an US pattern reflecting interstitial syndrome, all of whom ultimately had the diagnosis of pneumonia. In patients with initial abnormal CXRs, 17/18 had positive chest ultrasounds. The control arm did have 5/33 false positives which the author speculates may have been attributed to subclinical viral infections without clinical relevance or previous interstitial syndromes reflecting priorillness. The one false negative case was a patient with bacterial pneumonia with a deep, perihilar opacity.
The main limitation of this study is the small sample size and that the LUS studies were performed by expert sonographers. Beyond this though, we recognize that this study identified operating characteristics of LUS for all pneumonia and did not specifically analyze the sensitivity and specificity of lung ultrasound for viral pneumonia alone. It also excluded patients with comorbidities making this a very limited patient population which likely greatly affected the specificity of POCUS for pneumonia in this setting. Furthermore, expert adjudication was used to determine final diagnosis which is an imperfect gold standard. In the end, H1N1 has many similar characteristics to the COVID pandemic and this study is highly suggestive that lung ultrasound, particularly in patients with negative CXRs, can assist in diagnosis.
PMID: 22340202