A Neurointensivist’s Approach to POCUS for Increased ICP
Optic Nerve Sheath Dilation Occurs in Elevated ICP.
The optic nerves are encapsulated by a dural sheath arising from the meninges. Increases in intracranial pressure (ICP) are therefore transmitted to the CSF within the optic nerve sheath and result in dilation of the optic nerve sheath diameter.
Author: Dr. Tessa Damm - Clinical Adjunct Assistant Professor University of Wisconsin School of Medicine & Public Health - The POCUS Atlas Digital Education Fellow
Edited by Dr. Michael Macias, Temecula Valley Hospital; Dr. Matthew Riscinti, Denver Health Emergency Ultrasound
Introduction
The eyes are the window to the soul…
AND an accurate assessment of intracranial hypertension
As POCUS becomes more widely utilized in a variety of clinical settings, it is worth reviewing the utility of optic nerve sheath diameter (ONSD) in everyday clinical practice. Let’s face it, most non-neurologists are uncomfortable performing detailed neurologic evaluations. The eyes superficial location and fluid-filled nature render it an ideal target for POCUS. Couple this with the high sensitivity and specificity of ONSD and it becomes an obvious adjunct for patients presenting with headache, head trauma, altered mental status, or non-specific signs/symptoms that may otherwise be concerning for elevated ICP including somnolence and nausea/vomiting. As an intensivist specializing in both medical and neurocritical care, I utilize ONSD assessments in an analogous fashion to how I use whole body POCUS to rapidly differentiate the etiology of shock. ONSD quickly and seamlessly augments a basic neuro exam and differentiates whether a patients presentation is reflective of or concerning for elevated ICP.
My own clinical practice includes general medical and neurocritical care, where I have found the utility of ONSD assessment highest amongst patients outside of the neuro ICU when invasive neuro monitoring is either unavailable or contraindicated.
Basic tenants:
Technique
Use a linear transducer
Place patient in supine position
Place probe in transverse orientation
Closed eyelid (+/- tegaderm)
Assure on-axis view by concurrently imaging of lens
Position slightly laterally and angle inferomedially
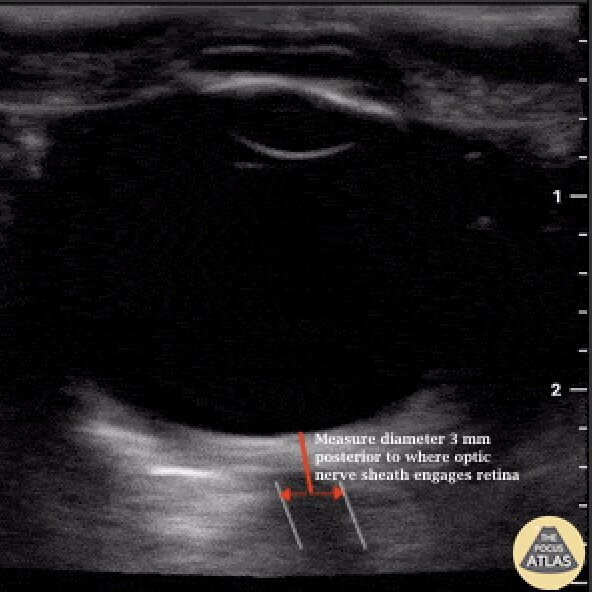
Measure diameter of optic nerve sheath 3 mm posterior to where optic nerve sheath engages retina
Repeat steps and use average of three measurements
Clinical Correlate
ONSD can be a useful non-invasive mechanism to monitor ICP over time. It is particularly useful if patient has relative contraindication to invasive ICP assessment, or if such monitoring is unavailable.
Pearls / Pitfalls:
If Tegaderm traps air over eyelid it will degrade view/image.
Off-axis measurements result in erroneous values.
Use “nerve” preset if your machine offers one.
Position transducer slightly laterally over globe with a subtle tilt in the inferomedial direction to gain best view of optic nerve.
If two linear hypo echoic structures are seen, it is the outer boarder which represents the optic nerve sheath (image below for example).
Patient Case
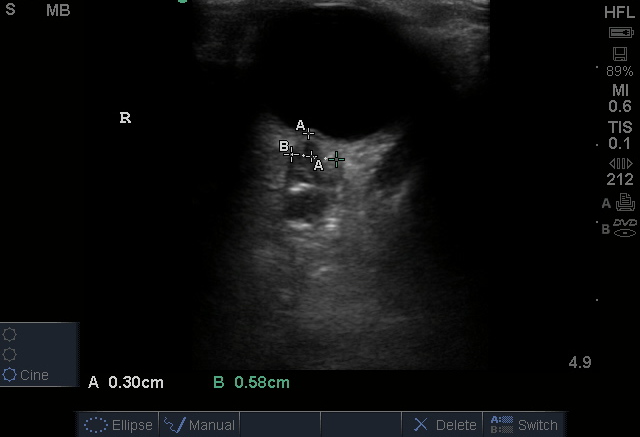
26 yo female with history of cerebral AVM presented with spontaneous intracranial hemorrhage with intraventricular hemorrhage (image above). Her clinical course was further complicated by development of refractory hypoxemia secondary to severe ARDS, warranting periodic prone positioning for management. Serial bedside ONSD measurements were instrumental in enabling a secondary assessment of ICP as invasive ICP measurements consistently appeared higher while she was in the prone position.
Seen here: MAP 89; ICP 28; CPP 61.
All images and case information used with patient permission.
Evidence Review: Controversies and Limitations
The largest systematic review and meta-analysis yielded quite promising operating characteristics. But what are the limitations of this knowledge?
PMID: 26112632
The Evidence Atlas previously reviewed this systematic review and meta-analysis:
Included 12 studies (n = 478).
ONSD cut point of 5 mm for adults.
4.5 mm for age 1–17 years, and 4 mm for age <1 year.
There was moderate to high heterogeneity among these studies given multiple patient populations.
The gold standard in this review was CT, which is a questionable gold standard compared to invasive ICP monitoring.
Overall their conclusions were that ocular sonography had a very low LR- (0.05) making it a good test for ruling out raised ICP in a low-risk group, and a high LR+ (12.4) making it a good test for ruling in raised ICP in a high-risk group.
How does ONSD compare to the gold standard of invasive intraparenchymal pressure monitoring?
A group in the Netherlands compared ONDS with intraparenchymal ICP measurement (4)
ONSD > 5.0 mm uniformly correlated with acute rise in ICP > 20 mm Hg
Correlation between ICP and ONSD was high (sensitivity 94%; specificity 98%; 95% CI 0.97-1.00)
A prior meta-analysis also compared ONSD with invasive ICP monitoring devices (2)
Why is there lack of uniform consensus re: optimal cutoff value for ONSD?
The elasticity of an individual’s optic sheath renders ONSD evaluation a qualitative rather than quantitative ICP assessment
A range of ONSD (4.8 mm to 5.9 mm) measurements, however, have been used to correlate with adult ICP >20 mm Hg
The ONSD Research Group is working through the minutiae to provide the world an optimized cutoff value
Until then, available meta-analyses have used a ONSD cutoff value of >5.0 mm and so should you
(3 & 2)
Remember that ICP is a dynamic rather than static measurement, subject to outside influences:
Maneuvers known to increase ICP including tracheal suctioning (4) and c-collar immobilization (7) accordingly result in acute increases ONSD
ONSD increases at high altitude and is associated with more severe symptoms of acute mountain sickness (8)
Much like systemic blood pressure, ICP is effected by patient positioning and level of activity. Not only is this a basic tenet in the practice of neurocritical care, it should be appreciated when performing serial ONSD measurements
Take Home
ONSD image acquisition is easy to learn, and quick to obtain.
The utility of non-invasive ICP assessment (of high sensitivity and specificity) is underrated and often overlooked. Like a majority of POCUS evaluations, ONSD is a useful adjunct that enables the astute clinician to direct timely and appropriate patient care. Consider incorporating it into your practice today!
More Images of ONSD Measurement
Learn More
View step-by-step instructional video at Core Ultrasound: https://www.coreultrasound.com/onsd/
References
Chesney GL, Mohabir PK. Ocular Ultrasound. In: Soni JN, Arntfield R, Kory P. Point-of-Care Ultrasound. Philadelphia, PA: Elsevier, 2015: 245-253.
Dubourg J, Javouhey E, Geeraerts T, et al. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2011;37:1059-1068.
Koziarz A, Sne N, Kegal F, et al. Bedside Optic Nerve Ultrasonography for Diagnosing Increased Intracranial Pressure: A Systematic Review and Meta-analysis. Ann Intern Med. 2019;171:896-905.
Maissan IS, Dirven PJAC, Haitsma IK, et al. Ultrasonographic measured optic nerve sheath diameter as an accurate and quick monitor for changes in intracranial pressure. J Neurosurg. 2015;123:743-747.
Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic Nerve Ultrasound for the Detection of Raised Intracranial Pressure. Neurocrit Care. 2011;15:506-515.
Ohle, R., McIsaac, S. M., Woo, M. Y., & Perry, J. J. (2015). Sonography of the Optic Nerve Sheath Diameter for Detection of Raised Intracranial Pressure Compared to Computed Tomography: A Systematic Review and Meta-analysis. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine, 34(7), 1285–1294.
Yard, J., Richman, P. B., Leeson, B., Leeson, K., Youngblood, G., Guardiola, J., & Miller, M. (2019). The Influence of Cervical Collar Immobilization on Optic Nerve Sheath Diameter. Journal of emergencies, trauma, and shock, 12(2), 141–144.
Sutherland, A. I., Morris, D. S., Owen, C. G., Bron, A. J., & Roach, R. C. (2008). Optic nerve sheath diameter, intracranial pressure and acute mountain sickness on Mount Everest: a longitudinal cohort study. British journal of sports medicine, 42(3), 183–188.