The Altered Infant - Should we POCUS an open fontanelle? A case of Hydrocephalus
Dr. Sathya Subramanian - Childrens Hospital of Philadelphia - Pediatric Emergency Ultrasound Fellow
Editors: Dr. Matthew Riscinti, Dr. Kyle Kelson, Dr. John Kilpatrick
It’s 7pm and a 3 month old is brought to you with inconsolable crying. According to the parents he’s been fussier for the past week, has been feeding less and is sleepier today. There have been no fevers, vomiting or diarrhea.
Vitals in the ED are HR 100, BP 110/70, saturation 100%, RR 36, Temp 37.4C. He is sleeping calmly in his mother’s arms.
The family says the pediatrician has scheduled an MRI for the child because of an increasing head circumference (> 100% head circumference, 80% length and weight) but the child has not yet received it. You are concerned and decide to start a sepsis workup while expanding your differential. You consider non-accidental trauma, toxin ingestion, a new metabolic diagnosis and intussusception. However, all the initial labs are normal. A quick POCUS exam of the abdomen reveals no intussusception.
Exam is grossly normal, except an anterior fontanelle that is wide, full and pulsatile.
https://www.bundoo.com/qotd/soft-spot-babys-head/
You realize the anterior fontanelle is open and full. The POCUS transducer could utilize this open window to visualize the brain. You decide this is a priority at this visit. His BP is high for age, his HC is more than 100% and he is sleepy. Is this an infant with an altered mental state?
You perform POCUS of the brain.
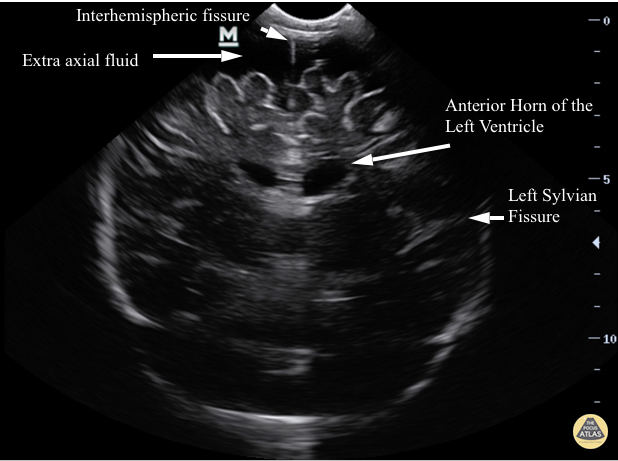
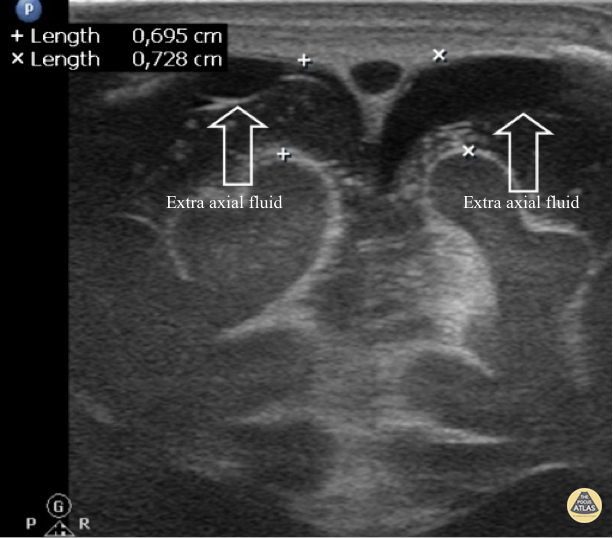
Clip 1: You notice significant enlargement of the extra axial space seen most clearly in the 12 o’clock position above the interhemispheric fissure.
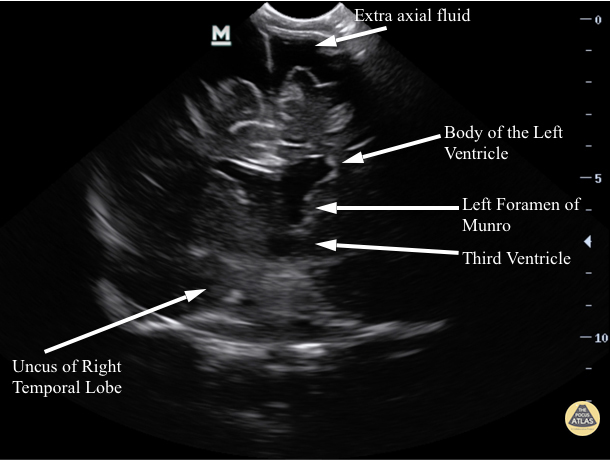
Clip 2: There is also asymmetry, specifically asymmetric ventricles with the left ventricle appearing larger than the right.
Although you are not facile with this particular POCUS modality, it is clear there is obvious asymmetry of the ventricles with the left ventricle appearing larger than the right. Furthermore, there is significantly increased extra-axial space seen most clearly in the 12 o’clock position above the inter-hemispheric fissure.
You decide this image needs more urgent imaging, order a CT head and consult neurosurgery while awaiting the results.
How can intracranial POCUS evaluate a pediatric patient?
1. Hydrocephalus (communicating, obstructive)
2. Intracerebral hemorrhage (intraventricular, subdural, intracerebral)
3. Infectious causes (meningitis, abscess)
Is there evidence that emergency physicians can use POCUS to visualize infant intracranial pathology?
The literature is mostly limited to case reports, but is worth considering, especially in an acutely life-threatening situations.
One published case involved an emergency physician using POCUS to not only visualize a subdural hematoma but also to drain the collection under ultrasound guidance through the open anterior fontanelle. This happened in the resuscitation bay while this infant was actively herniating! (1)
A second case involved an emergency physician diagnosing severe intraventricular hemorrhage as the cause for acute seizures and anemia in a 16-day-old infant (2). Additional cases support using POCUS to visualize the ventricles, aiding in the diagnosis of hydrocephalus (3,4).
Intracranial infections are less commonly visualized with the ultrasound, but is possible, with one case report (5) and a published review article from a radiology group highlighting the various sonographic features of early neonatal meningitis, ventriculitis, brain abscess and subdural empyema (6). Some of these highlighted sonographic findings in the article include increased echogenicity and thickness of the sulci, hyperechoic debris within the ventricles or subdural space, and discrete hypoechoic collections within the brain parenchyma.
How is the intracranial POCUS scan performed?
The emergency physician performing the POCUS scan can either use a phased array, neonatal or even the endocavitory probe. All of these have the same frequency (4 – 9MHz) and can be placed directly on the open anterior fontanelle. The transducer is used to visualize the brain in 2 planes, coronal (Clip 3) and sagittal (Clip 4).
Clip 3: The coronal plane has the indicator marker to the right and is placed on the anterior fontanelle. The ultrasound beam is swept from the anterior to posterior aspect of the head.
Clip 4: The sagittal plane has the indicator marker facing the anterior aspect of the face and the ultrasound beam is swept in either the left to right or right to left direction of the patient’s shoulders.
Ideally the intracranial POCUS scan should then be completed with a linear transducer placed over the anterior fontanelle in the coronal and sagittal orientation. Utilizing its high frequency, the operator should attempt to visualize the superior sagittal sinus above the interhemispheric fissure and examine the superficial surface of the brain for any signs of extra axial fluid. This is a particularly difficult view but an important area to visualize as subdural hematomas can be seen in this region.
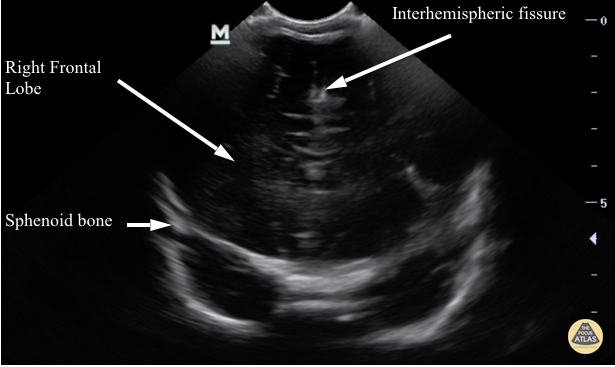
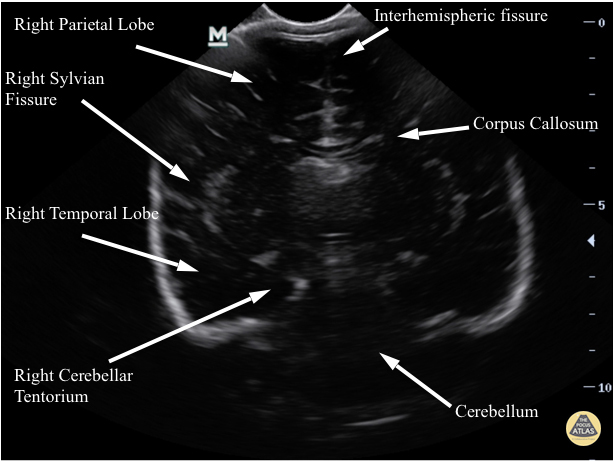
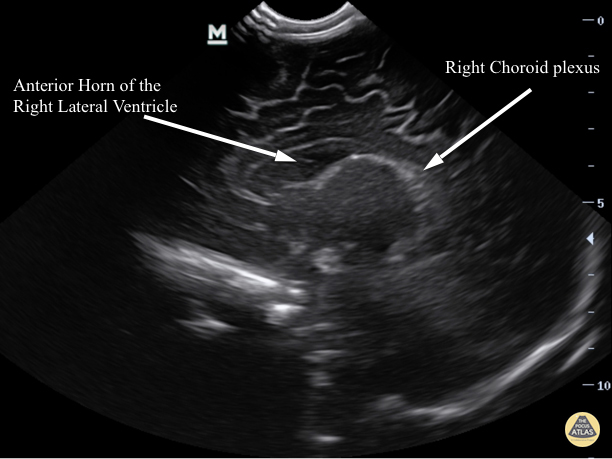
What anatomy can be used as landmarks?
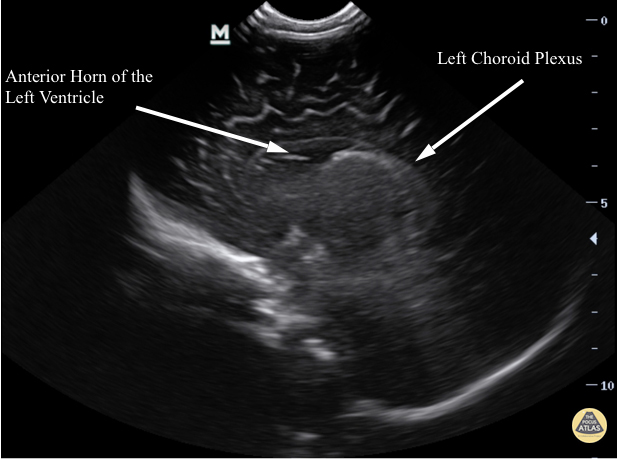
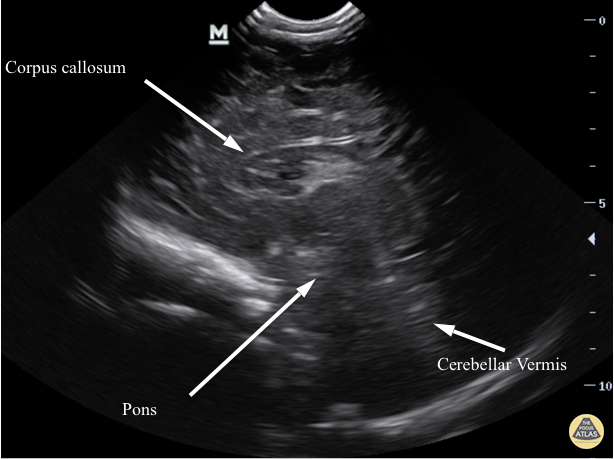
Intracranial POCUS is different from the comprehensive brain ultrasound performed by sonographers as the questions we ask are different. Is there evidence of hydrocephalus? Are there signs of intraventricular or intracranial hemorrhage? Are there signs of infection? Thus, the landmarks used in POCUS are primarily used to ensure that adequate views have been obtained. Scroll through our labeled still library below.
Case Resolution
Following the intracranial POCUS on our patient, there was concern for an enlarged, asymmetrical left ventricle with significant extra axial fluid. The infant subsequently had a CT head in the ED, was admitted to the PICU and an MRI brain as an inpatient that confirmed symmetrical ventriculomegaly with prominent but benign appearing CSF fluid layering the subdural space. The combination of the infant’s imaging and clinical appearance was concerning for potential early obstructive hydrocephalus with increased extra axial space. The infant continues to be followed by the neurosurgical service and is being clinically monitored as an outpatient for any delay in achieving his developmental milestones, along with other parameters like head circumference and weight gain.
See more of our Pediatrics cases in our Pediatric Atlas.
References
Lee S, Bellamkonda Athmaram VR, Anderson JL. Infant with limpness; subdural hemorrhage from suspected abusive head trauma. Ann Emer Med. 2013; 61(1):18,36
Halm BM, Franke AA. Diagnosis of an intraventricular hemorrhage by a pediatric emergency medicine attending using point-of-care ultrasound: a case report. Pediatr Emerg Care. 2011; 27(5): 425-7
Yaeger SK, Marin JR. An infant diagnosed with hydrocephalus by point-of-care ultrasound. Pediatr Emerg Care. 2017; 33(4): 287-289
Doctor K, Cohen JS. Diagnosis of an intraventricular cyst using point-of-care cranial ultrasound in the pediatric emergency department. Pediatr Emerg Care. 2017; 33(3):216-218
Ahmad S. Kampondeni S, Molyneux E. An experience of emergency ultrasonography in children in a sub-saharan setting. Emerg Med J. 2006; 23(5): 335-40
Gupta N, Grover H, Bansal I, et al. Neonatal cranial sonography: ultrasound findings in neonatal meningitis –a pictoral review. Quant Imaging Med Surg. 2017; 7(1): 123-131