Pulmonary Evidence
POCUS Evidence Atlas - Pulmonary. EBM review and resource of POCUS for pulmonary diagnoses. Sensitivity Specificity positive and negative likelihood ratios.
The Evidence Atlas: Pulmonary
Jump To Clinical Application: Pulmonary Edema Pneumothorax Pleural Effusion Pneumonia
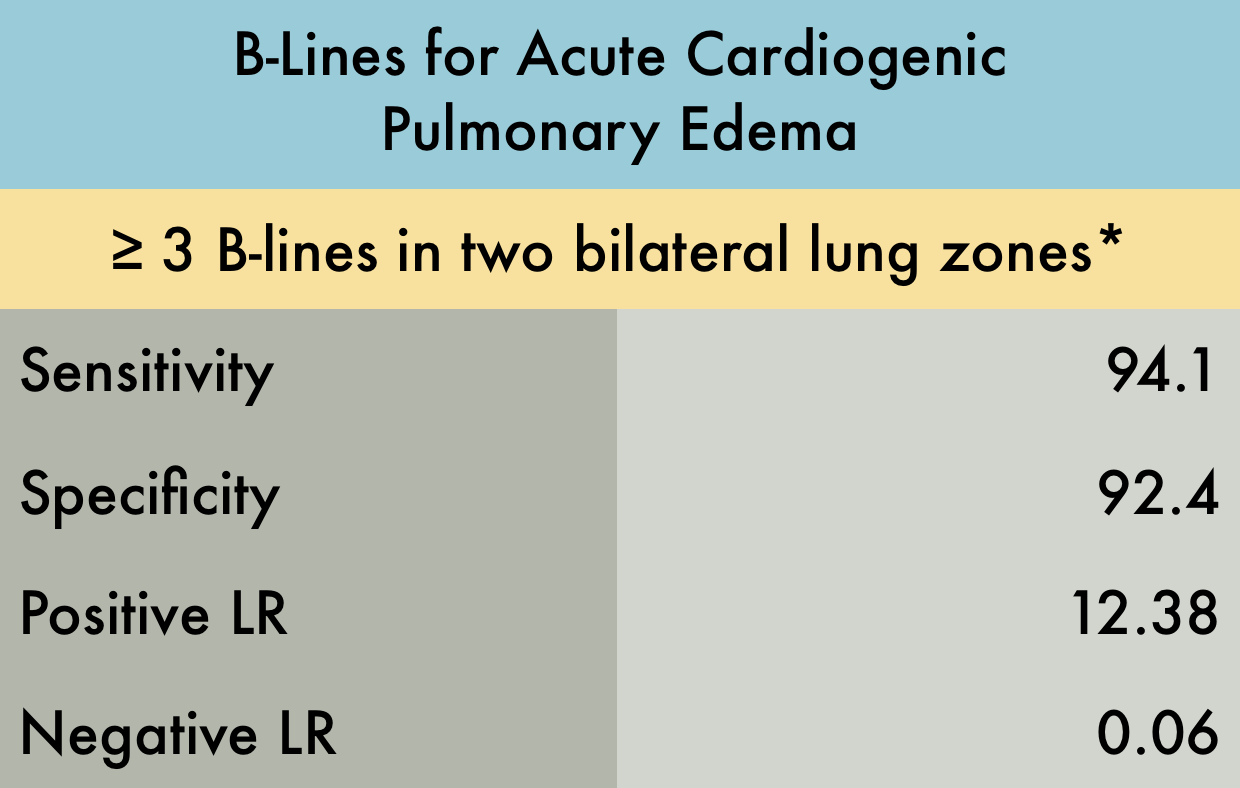
Pulmonary Edema
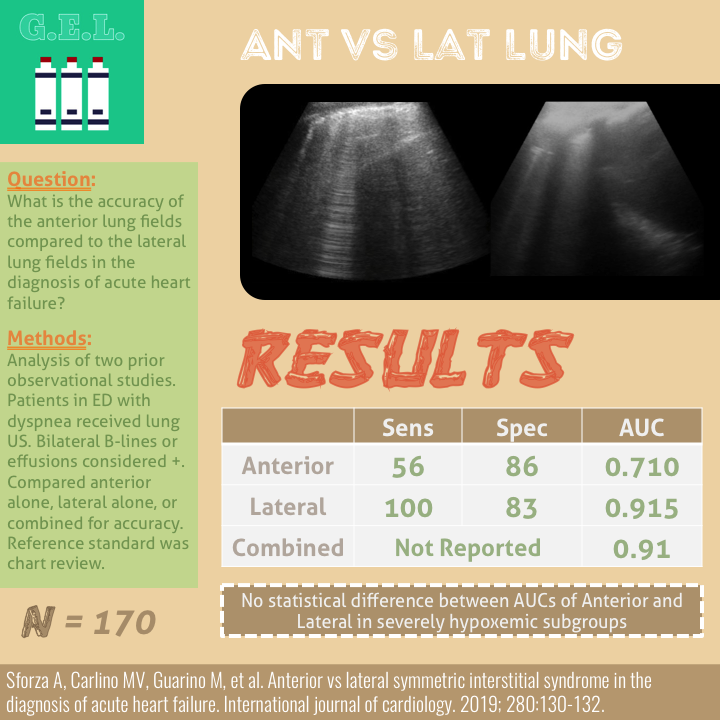
This was a systematic review including 7 prospective case control or cohort studies (n=1075) evaluating the sensitivity and specificity of B-lines in diagnosing acute cardiogenic pulmonary edema (ACPE). The included studies recruited patients presenting to the hospital with acute dyspnea, or where there was a clinical suspicion of congestive heart failure. The setting was either the emergency department (ED) , ICU, or inpatient wards. Ultrasound examinations were performed by any non-radiologist physician. *Various lung ultrasound protocols were used, including the Volpicelli method, the Lichtenstein protocol, and the Comet Score. All involved using B-lines to make the diagnosis of ACPE. The varied protocols used for diagnosis may explain the increased sensitivity noted in this study compared to other meta-analysis. Gold standard was heterogeneous amongst studies with 'final diagnosis from clinical follow-up' being an acceptable reference standard.
PMID: 25176151
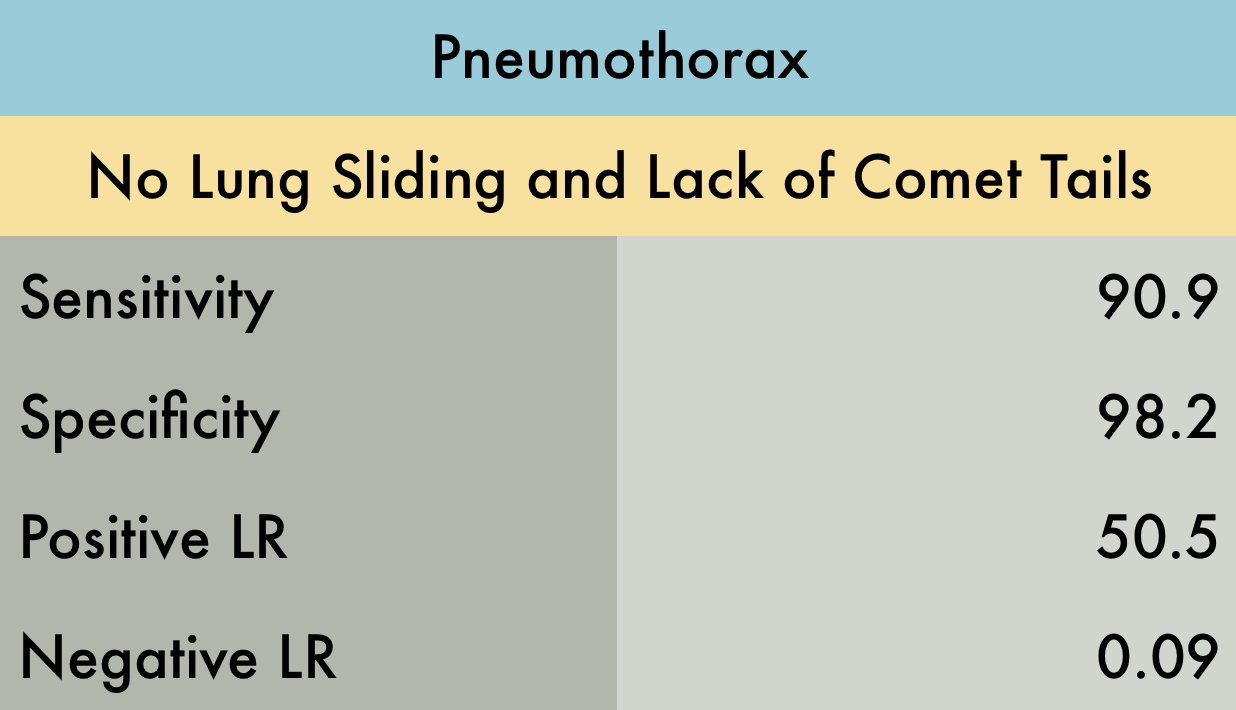
Pneumothorax
This was a systematic review of 8 prospective studies (n=1048) of adult patients. Included manuscripts evaluated for traumatic or iatrogenic pneumothorax. No studies that screened for spontaneous pneumothorax were included. Examiners were surgeons, radiologists, or emergency providers. Reference standard was pneumothorax found on CT or a rush of air upon tube thoracostomy. All studies but one used the ultrasonographic signs of lung sliding and comet tail to rule out pneumothorax. Although the exact technique used to perform the ultrasound examination is not reported with enough detail in some studies, most agree on requiring the examination of more than one intercostal space in both the midclavicular line and laterally and inferiorly at the anterior or midaxillary lines. Lastly, this data does not evaluate whether the pneumothoraces identified were clinically significant.
PMID: 21868468
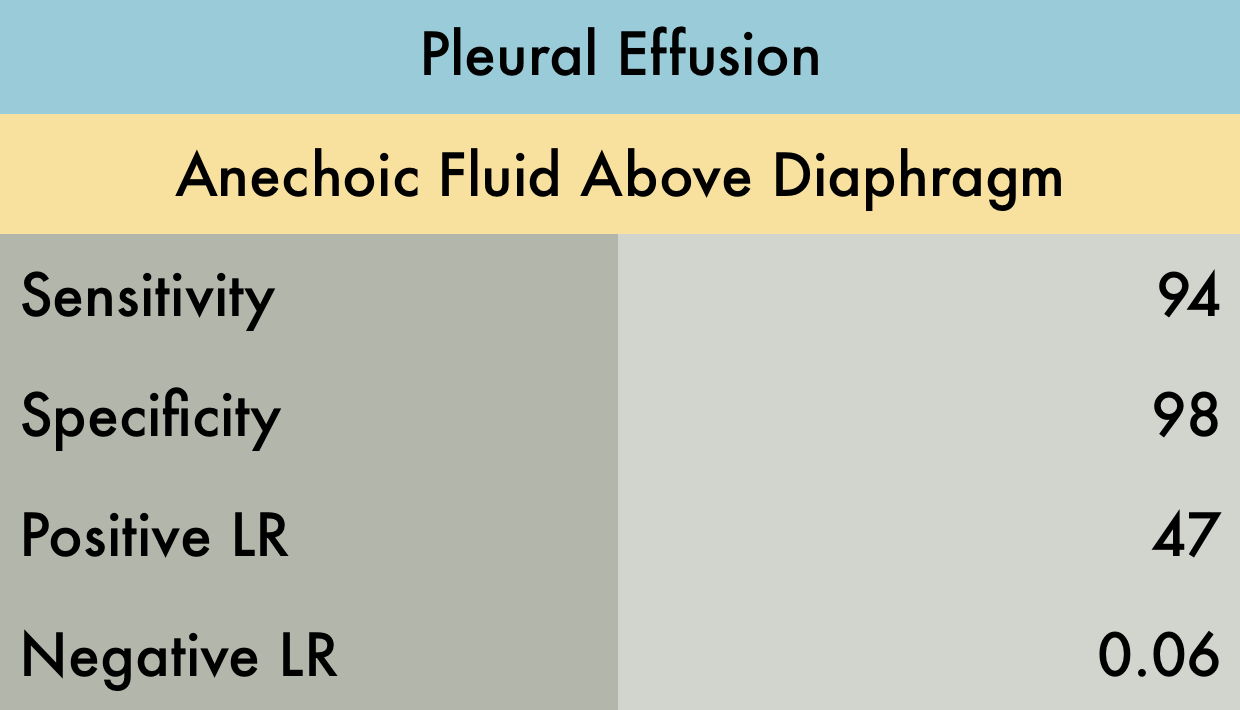
Pleural Effusion
This was a meta-analysis including 12 retrospective and prospective studies (n=1554) of adults and pediatric patients. Ultrasound was used to diagnose pleural effusion, with the reference standard either CT, surgery, or a more formal “high quality ultrasound in conjunction with expert end diagnosis.” Ultrasound examinations were performed by a variety of operators including emergency physicians, intensivists, radiologists, and nurses. Exact criteria for diagnosis of a pleural effusion by ultrasound was not defined.
PMID: 26862542
Pneumonia
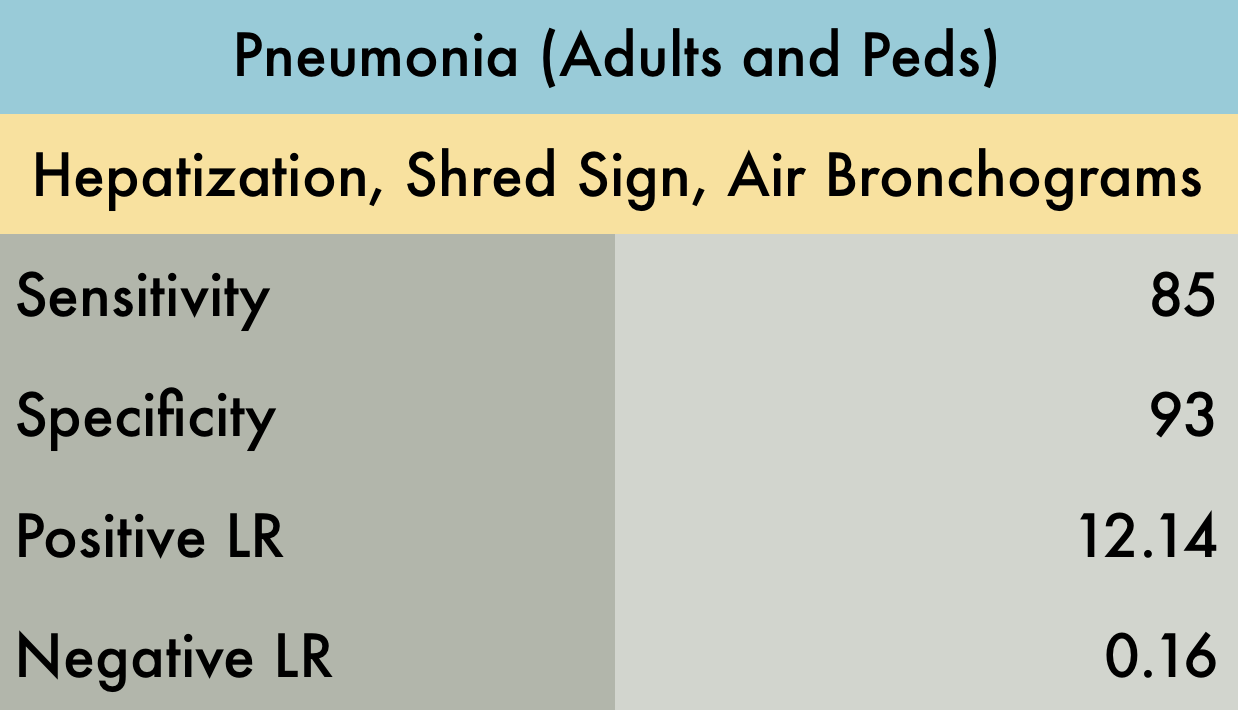
The was a systematic review including 20 prospective adult and pediatric studies (n=2513) with varied settings including the emergency department, inpatient wards, or ICU. A positive finding on ultrasound was identified as an alveolar and interstitial pattern or consolidation, although this is not further expanded upon. Gold standard was either CT, chest radiography, or “clinical diagnosis” depending on the study. One large caveat of this study is that it has a very large degree of heterogeneity, with ultrasound examinations performed by emergency physicians, intensivists, and radiologists of varying levels of expertise, on patients ranging from ambulatory to critically ill.
PMID: 28244009
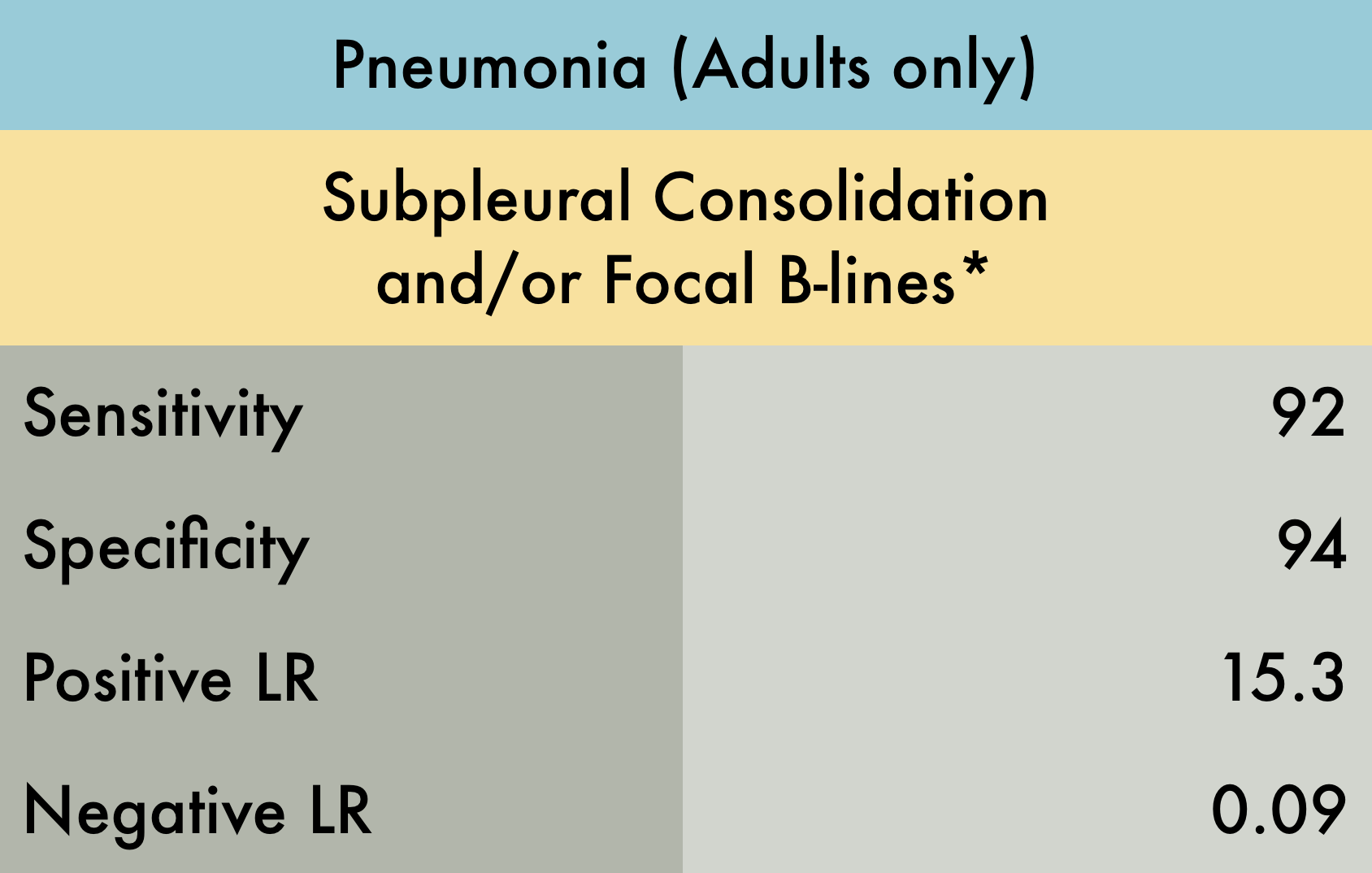
This was a systematic review including 17 prospective studies (n=5108) evaluating the operating characteristics of lung ultrasound for pneumonia in adult patients seen in the emergency department with a clinical suspicion for this diagnosis. Reference standard was either chest radiograph, chest CT, or final clinical diagnosis. Included studies varied with regards to which and how many lung fields were evaluated. The operators performing ultrasound examinations were exclusively emergency physicians or radiologists.*Subpleural consolidation and/or focal B-lines were the diagnostic criteria in the majority of manuscripts included, however in 4 studies, no clear positive findings were specified.
PMID: 29189351
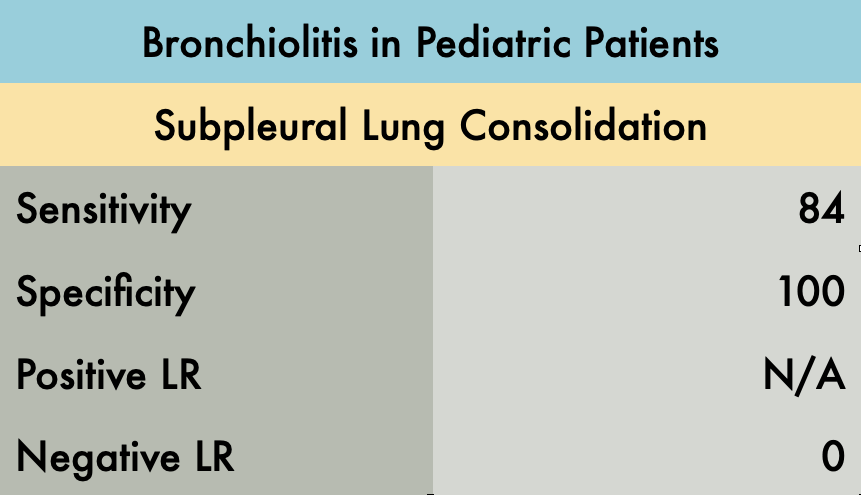
This was a prospective observational study comparing the operating characteristics of emergency department (ED) performed LUS versus CXR for diagnosis of children with bronchiolitis. A total of 52 patients were enrolled in the study. All LUS were performed by one blinded experienced sonographer. Abnormal LUS findings in the study included: subpleural consolidations, b-lines (confluent b-lines or areas of multiple b-lines), and pleural abnormalities. In 44/52 infants with bronchiolitis, subpleural consolidations were present, compared to 0/52 infants without bronchiolitis. Notably, the sensitivity increased from 84% to 90% when all LUS abnormalities are considered (b-lines and pleural irregularities in addition to subpleural consolidation). The presence of multiple areas of lung consolidation and confluent b-lines (white lung) were most predictive of the bronchiolitis severity. CXR was considered positive in 38/52 patients when lung consolidation, peribronchial thickening, or hyperexpansion was identified. Nine patients with a negative CXR but abnormal LUS findings had a clinical course that was consistent with bronchiolitis.
An advantage of LUS in this study was decreased time to diagnosis. LUS was interpreted during the study, while CXR took an average of 4 hours and 45 minutes to interpret after imaging was obtained. Limitations of this study include the small sample size and a single operator for all ultrasounds performed. Bronchiolitis is typically a clinical diagnosis and as such was defined by history and clinical examination in this study. The current study compared LUS to CXR, but there is no gold standard for diagnosing bronchiolitis.. These limitations make the specificity of 100% questionable and indicate the need for larger studies.
PMID: 21468639
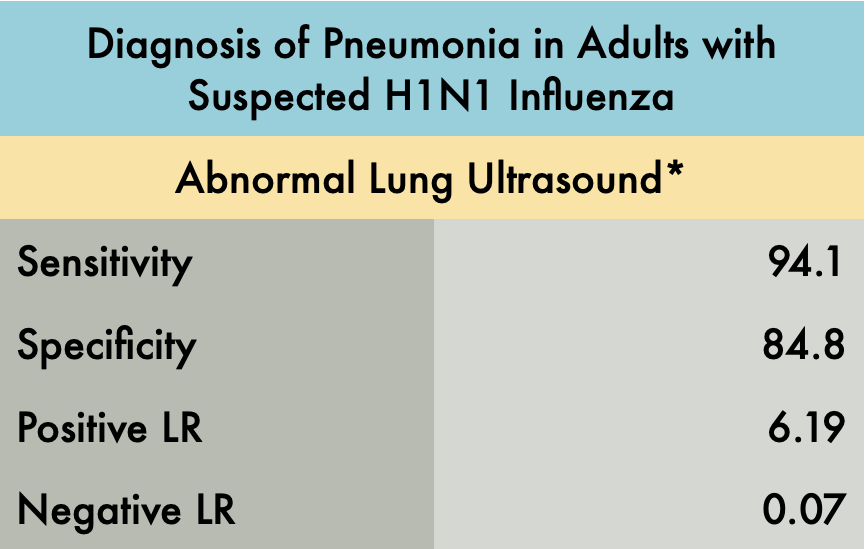
This was a prospective observational study comparing the operating characteristics of emergency department (ED) performed LUS versus CXR for the diagnosis of pneumonia in patients with suspected H1N1 influenza. The operating characteristics described in the table include patients with any pneumonia: primary bacterial pneumonia, viral (H1N1) pneumonia, or a secondary bacterial pneumonia in H1N1 infected patients. Patients were included in the experimental arm if they had signs or symptoms of influenza-like illness (ILI) with suspicion of lung involvement (pneumonia), either bacterial or viral. A total of 87 patients were enrolled in the study, 41 with ILI with suspected pneumonia and 46 with ILI without suspected pneumonia (control group).
The gold standard final diagnosis of pneumonia was based on the chart review of the hospital course including the history, physical exam, lab results, and radiographic findings. The reviewers were blinded to the LUS results. Three outcomes were reported: viral pneumonia with laboratory confirmation of the H1N1, primary bacterial pneumonia, or secondary bacterial pneumonia with confirmed H1N1.
The LUS studies were performed by three different emergency physicians with greater than 10 years of ultrasound experience. This study evaluated each hemithorax in five areas: two anterior, two lateral, and one posterior. The presence of any of the following signs on LUS indicated an abnormal exam*:
>3 B-lines per intercostal space
Thickness of pleural line > 2mm or coarse appearance
Consolidation or hepatization
Pleural effusion
Lung ultrasound showed a sensitivity of 94.1% and specificity of 84.8%. An abnormal ultrasound was present in 32 of 34 patients with the ultimate diagnosis of pneumonia (including viral and bacterial). In patients with initially negative CXRs, 15/16 demonstrated an US pattern reflecting interstitial syndrome, all of whom ultimately had the diagnosis of pneumonia. In patients with initial abnormal CXRs, 17/18 had positive chest ultrasounds. The control arm did have 5/33 false positives which the author speculates may have been attributed to subclinical viral infections without clinical relevance or previous interstitial syndromes reflecting priorillness. The one false negative case was a patient with bacterial pneumonia with a deep, perihilar opacity.
The main limitation of this study is the small sample size and that the LUS studies were performed by expert sonographers. Beyond this though, we recognize that this study identified operating characteristics of LUS for all pneumonia and did not specifically analyze the sensitivity and specificity of lung ultrasound for viral pneumonia alone. It also excluded patients with comorbidities making this a very limited patient population which likely greatly affected the specificity of POCUS for pneumonia in this setting. Furthermore, expert adjudication was used to determine final diagnosis which is an imperfect gold standard. In the end, H1N1 has many similar characteristics to the COVID pandemic and this study is highly suggestive that lung ultrasound, particularly in patients with negative CXRs, can assist in diagnosis.
PMID: 22340202