Orbital Evidence
POCUS Evidence Atlas - ocular eye and orbit. intracranial pressure. EBM review and resource of POCUS for echo diagnosis. Sensitivity Specificity positive and negative likelihood ratios.
The Evidence Atlas: Orbital
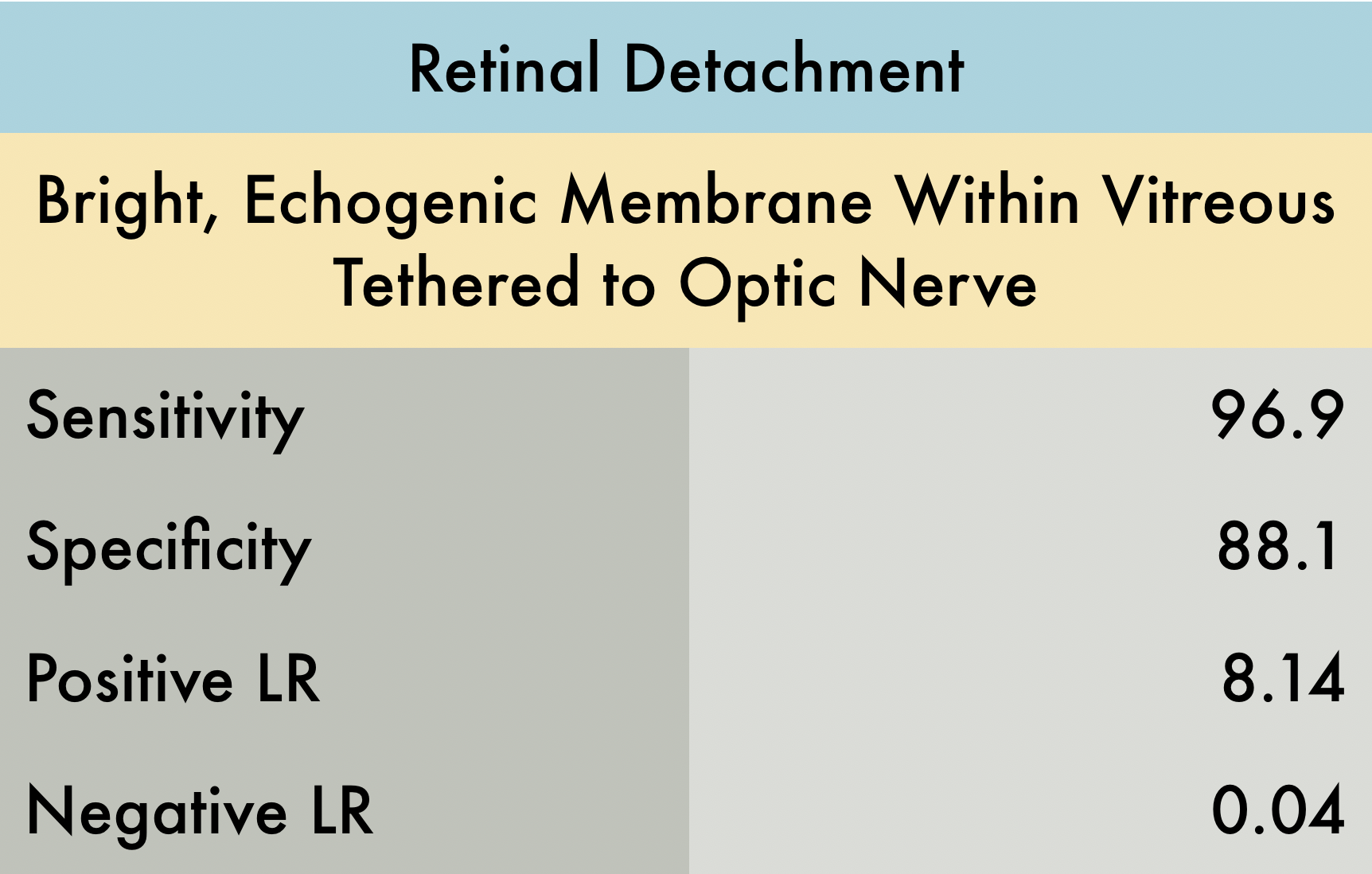
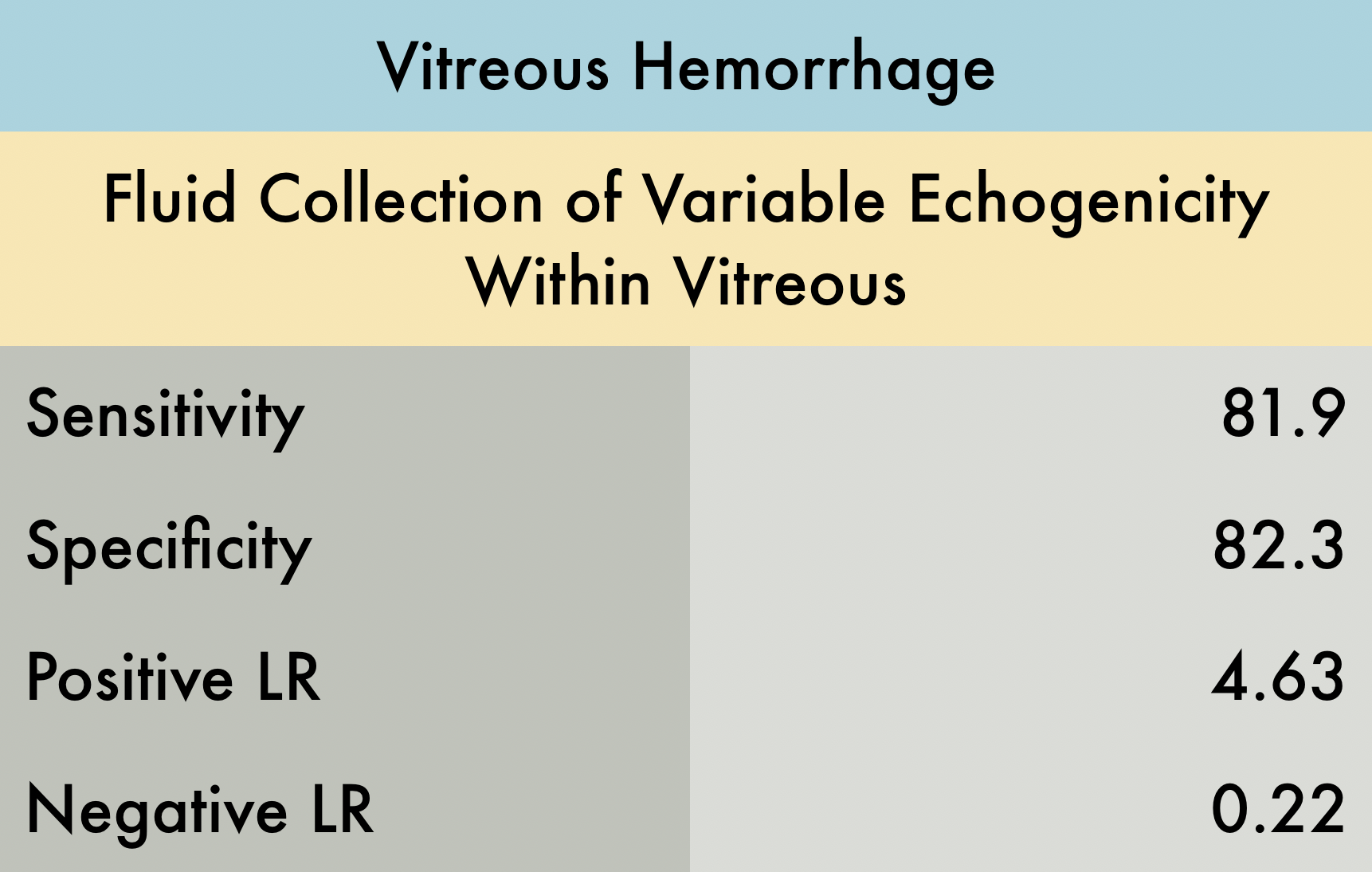
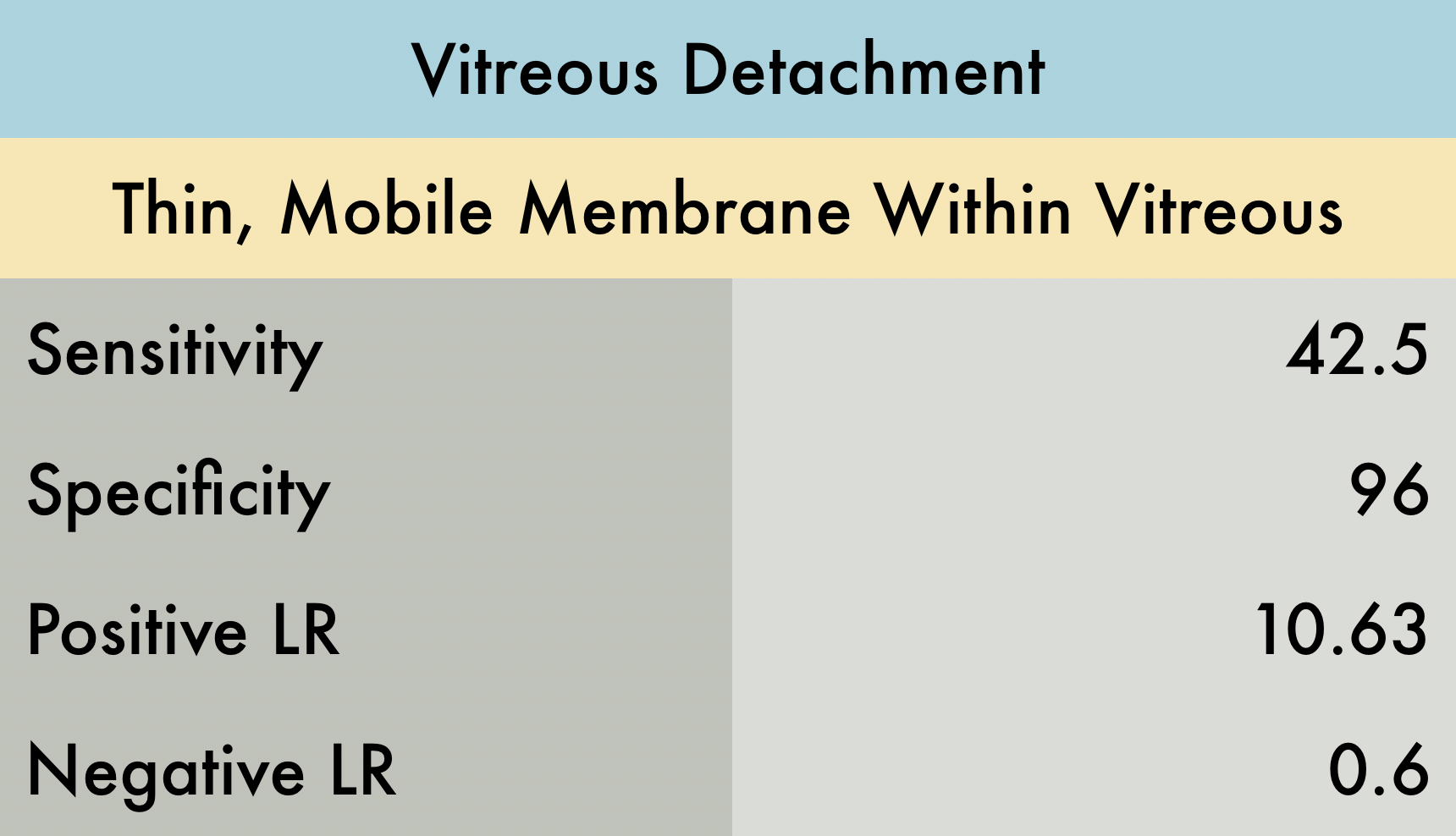
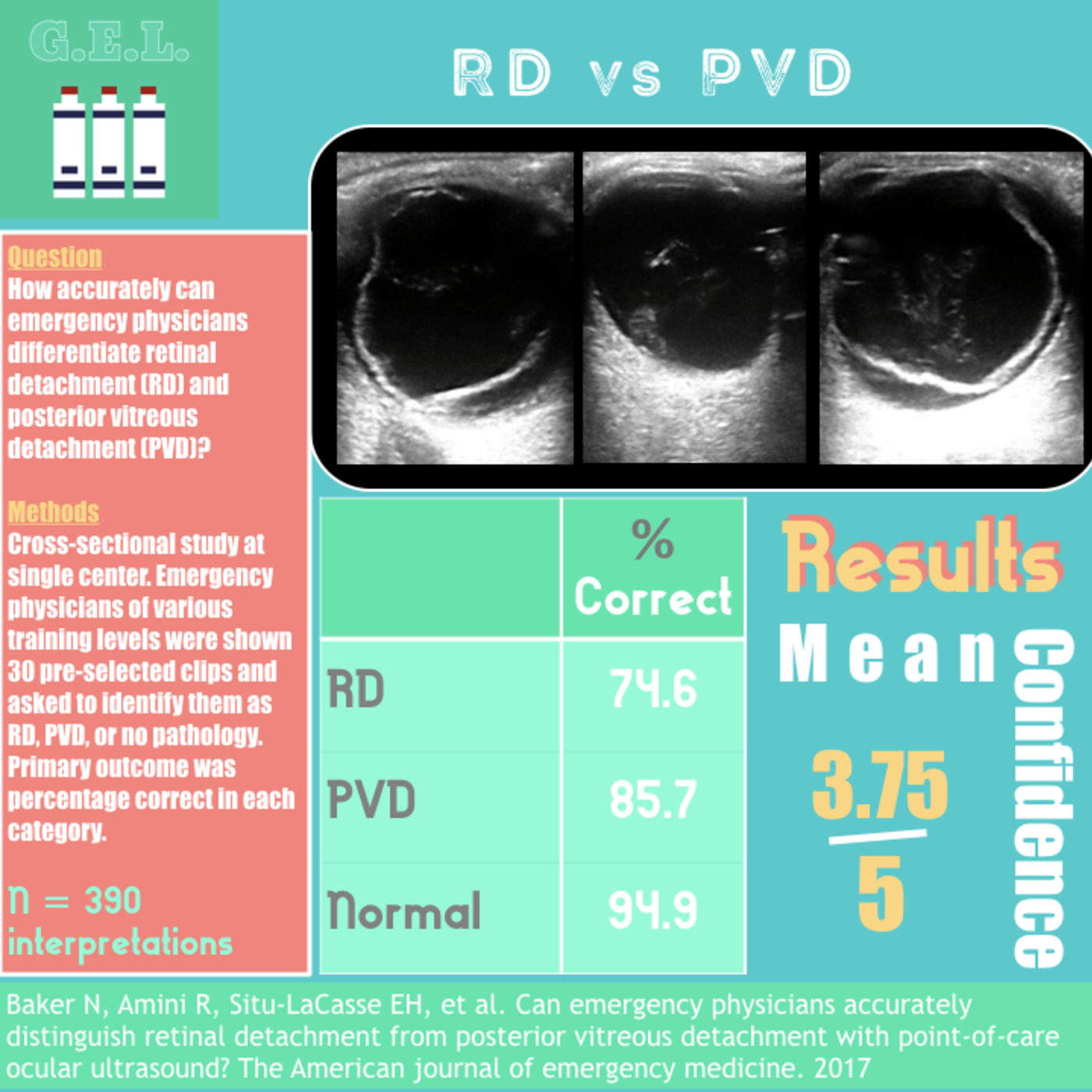
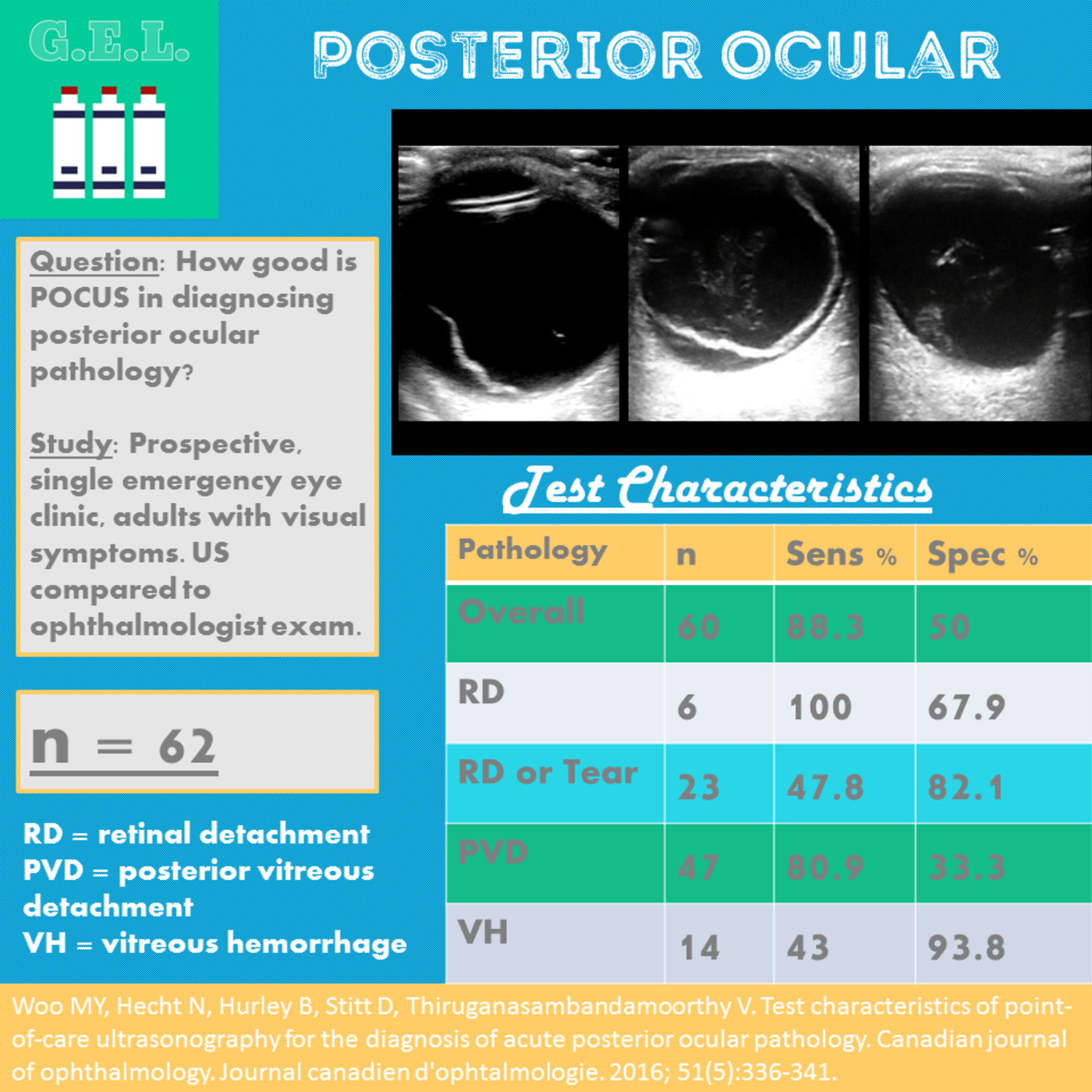
This was a prospective, multi-center study conducted at 2 academic emergency departments (ED) and 2 county hospital EDs (n = 225) to evaluate the accuracy of POCUS for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD). Each hospital recruited patients presenting to the ED with symptoms of blurry vision, flashers/floaters, and vision loss, whom required emergent ophthalmologic consultation; patients with ocular trauma or suspected globe rupture were excluded. Reference standard was attending ophthalmologists’ final diagnosis masked to POCUS results. Exams were performed by seventy-five unique providers including seventy emergency physicians of varying training level and 5 physician assistants. Study findings demonstrate that the utility of ED POCUS in the diagnosis for RD and VH were quite sensitivity and specific. The utility of POCUS in the diagnosis of VD was less sensitive (42.5%) but remained specific (96%). Overall, ocular POCUS by ED providers is a very good test to both rule-in and rule-out the emergent diagnosis of RD. The use of ocular POCUS is not as good of a test to rule-in or rule-out less emergent diagnoses of VD and VH but provides useful adjunct information to support evidence for those diagnoses. PMID: 30977855 - Reviewed by Dr. Jaclyn Walker
This was a prospective, multi-center study conducted at 2 academic emergency departments (ED) and 2 county hospital EDs (n = 225) to evaluate the accuracy of POCUS for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD). Each hospital recruited patients presenting to the ED with symptoms of blurry vision, flashers/floaters, and vision loss, whom required emergent ophthalmologic consultation; patients with ocular trauma or suspected globe rupture were excluded. Reference standard was attending ophthalmologists’ final diagnosis masked to POCUS results. Exams were performed by seventy-five unique providers including seventy emergency physicians of varying training level and 5 physician assistants. Study findings demonstrate that the utility of ED POCUS in the diagnosis for RD and VH were quite sensitivity and specific. The utility of POCUS in the diagnosis of VD was less sensitive (42.5%) but remained specific (96%). Overall, ocular POCUS by ED providers is a very good test to both rule-in and rule-out the emergent diagnosis of RD. The use of ocular POCUS is not as good of a test to rule-in or rule-out less emergent diagnoses of VD and VH but provides useful adjunct information to support evidence for those diagnoses. PMID: 30977855 - Reviewed by Dr. Jaclyn Walker
This was a prospective, multi-center study conducted at 2 academic emergency departments (ED) and 2 county hospital EDs (n = 225) to evaluate the accuracy of POCUS for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD). Each hospital recruited patients presenting to the ED with symptoms of blurry vision, flashers/floaters, and vision loss, whom required emergent ophthalmologic consultation; patients with ocular trauma or suspected globe rupture were excluded. Reference standard was attending ophthalmologists’ final diagnosis masked to POCUS results. Exams were performed by seventy-five unique providers including seventy emergency physicians of varying training level and 5 physician assistants. Study findings demonstrate that the utility of ED POCUS in the diagnosis for RD and VH were quite sensitivity and specific. The utility of POCUS in the diagnosis of VD was less sensitive (42.5%) but remained specific (96%). Overall, ocular POCUS by ED providers is a very good test to both rule-in and rule-out the emergent diagnosis of RD. The use of ocular POCUS is not as good of a test to rule-in or rule-out less emergent diagnoses of VD and VH but provides useful adjunct information to support evidence for those diagnoses. PMID: 30977855
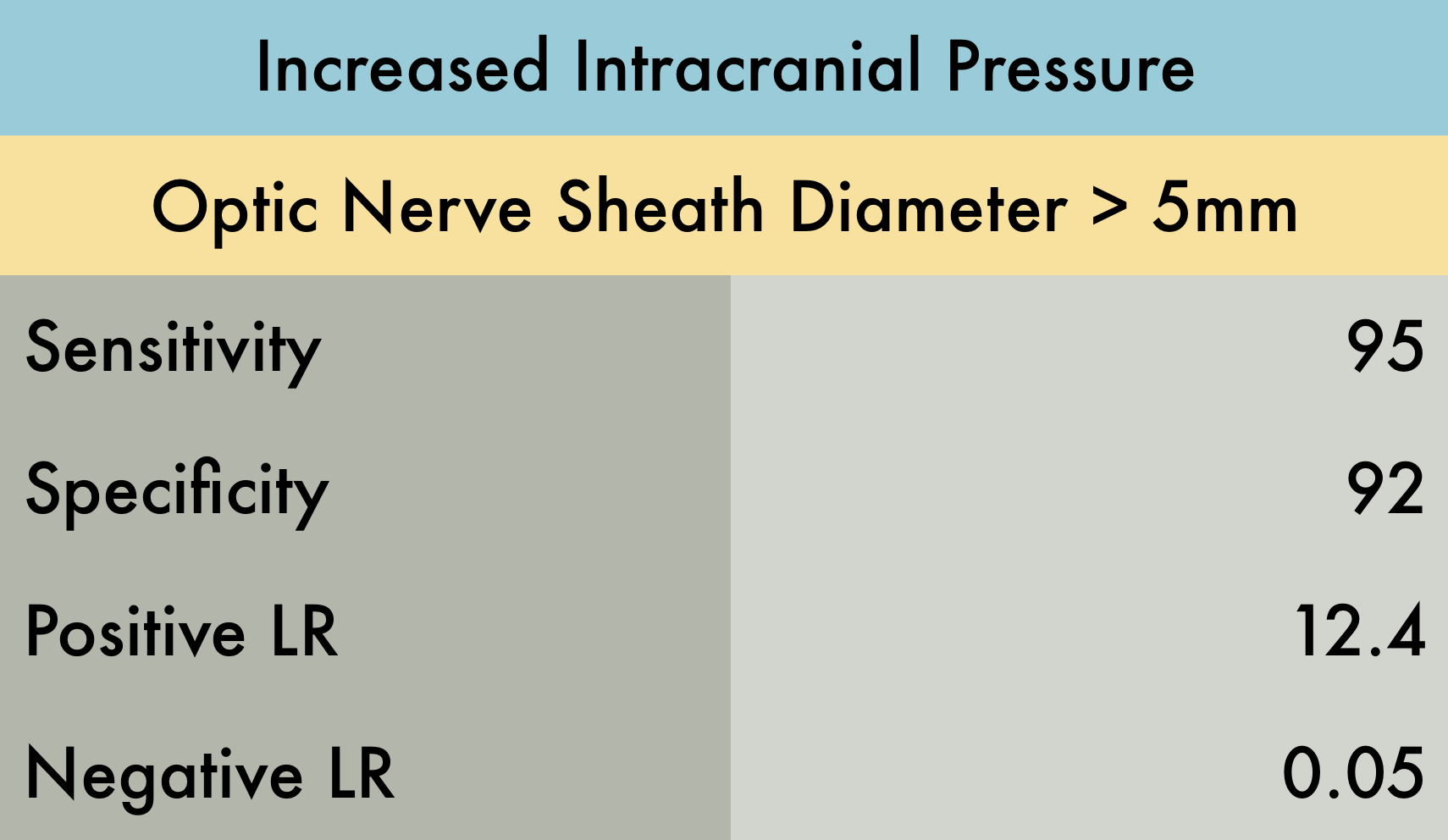
This was a systematic review, which including 12 studies (n = 478) using ultrasound measurement of optic nerve diameter (cut point of 5 mm for adult studies, 4.5 mm for age 1–17 years, and 4 mm for age <1 year) to evaluate for increased intracranial pressure (ICP). There was moderate to high heterogeneity among these studies given multiple patient populations. This resulted in wide confidence intervals: sensitivity of 95.6% (95% CI, 87.7%–98.5%), specificity of 92.3% (95% CI, 77.9%–98.4%), positive likelihood ratio of 12.5 (95% CI, 4.2–37.5), and a negative likelihood ratio of 0.05 (95% CI 0.016–0.14). It is also important to mention that the gold standard in this review was CT, which is not as accurate as invasive ICP monitoring. Overall their conclusions were that ocular sonography had a very low LR- (0.05) making it a good test for ruling out raised ICP in a low-risk group, and a high LR+ (12.4) making it a good test for ruling in raised ICP in a high-risk group.
PMID: 26112632